Can I exercise after an angioplasty and stent? Absolutely yes!
Having worked many years in a hospital-based cardiac rehab unit as well as in private clinics, I have heard nearly every question about what to do after an angioplasty.
In this 2025 updated article, I deep dive into these questions, explain everything in simple terms (no jargon), and deliver the best, most comprehensive resource to help you regain your health fitness!
For my math-challenged friends, I’ve gone the extra mile and embedded a super simple exercise heart rate calculator, so you don’t even need to leave the page.
Finally, don’t miss the 350+ reader comments at the end where readers can ask questions and share their inspiring stories of recovery.
- What is angioplasty?
- What is a stent?
- Angioplasty / stent images
- Cardiac medications
- Lifestyle changes
- Benefits of exercise
- Post-operative exercise risk
- Can exercise damage the stent?
- When can I exercise after angioplasty and stent?
- Aerobic exercise after angioplasty
- Determining exercise heart rate
- Lifting weights after angioplasty
- Stretching and flexibility training
- Playing sports after angioplasty
- Take home message
To get started, you must first understand a few important background concepts:
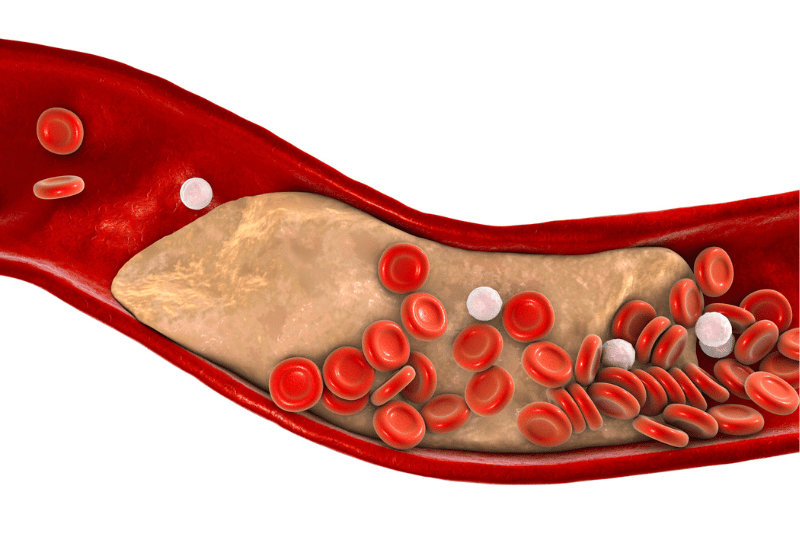
- Coronary artery disease (CAD) causes narrowing of the blood vessels that feed blood to your heart muscle.
- CAD can cause angina (i.e., pain and/or pressure in the chest, neck, back, jaw, arms).
- Untreated angina may progress to a complete blockage (arterial occlusion) and lead to a heart attack (myocardial infarction).
- A cardiac catheterisation is usually performed to determine the extent of the blockages and help the doctor decide if an angioplasty is necessary and if a stent should be placed.
What is angioplasty?
The term angioplasty comes from the Greek words angio meaning “vessel” and plastia meaning “fit for moulding” but really it’s just a fancy name for a cardiac plumbing job.
The full name for the procedure is percutaneous transluminal coronary angioplasty (PTCA) or percutaneous intervention (PCI)
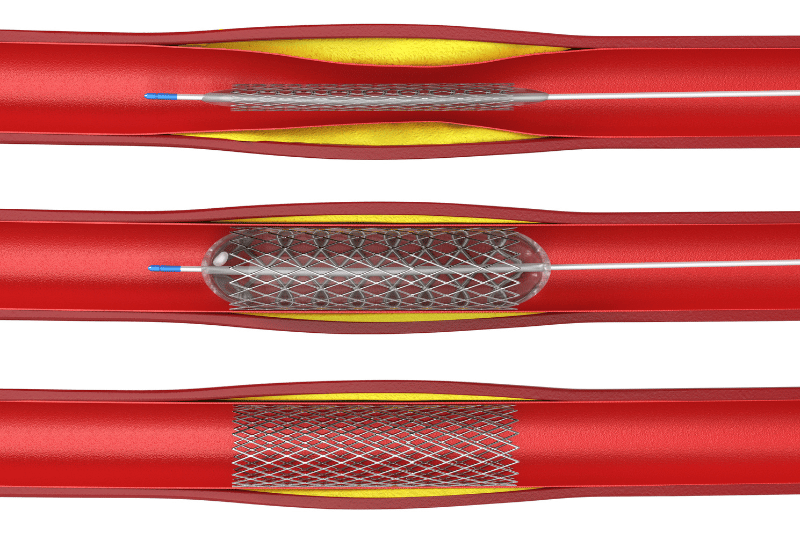
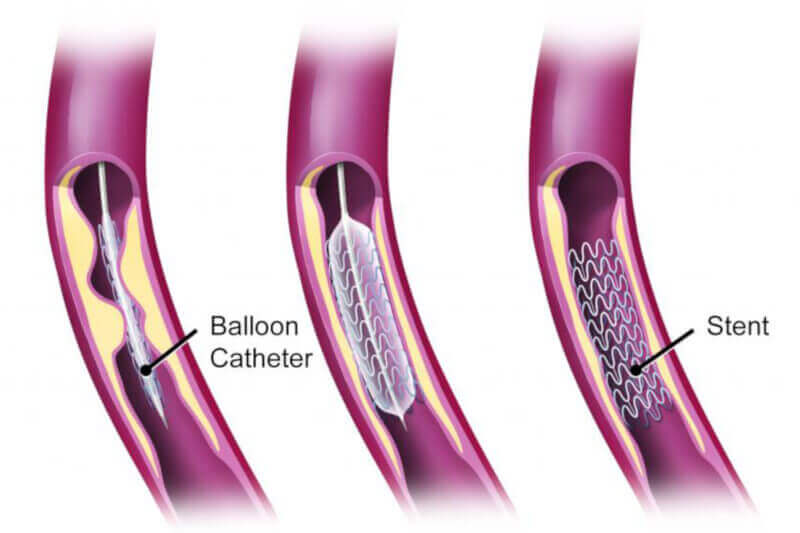
Translation: percutaneous means they pass an inflatable catheter through the skin (at your femoral artery in your groin area) traveling through the lumen (the space within your artery), up into your aorta, and then enter into your coronary blood vessels (the arteries that serve blood to the heart). Once the blockage is spotted, the doctor then passes the catheter into the blockage and inflates a small balloon to expand the blood vessel and reestablish blood flow.
What is a stent?
Sometimes a stent is inserted during the angioplasty procedure.
A stent is a little wire mesh which keeps the artery open after the balloon has been removed and minimises the chance of the artery blocking up again (restenosis).
The two main types of stents include a bare metal stent and a drug-eluting (medicine-coated) stent, the latter of which helps prevent scar tissue from blocking the artery. Interestingly, recent research shows that newer drug-eluting stents are associated with a lower mortality, fewer redo procedures on the same artery, and fewer heart attacks, and are preferred over bare metal stents during angioplasty.
Angioplasty / stent images
During an angioplasty procedure, a balloon catheter with a stent is inserted into the blocked artery before it is inflated to push the plaque out of the way. Once inflated, the catheter and balloon are removed, leaving the stent in place with reestablished arterial blood flow.
Cardiac medications
Cardiac medications are commonly prescribed to help minimise the risk of your artery blocking up again (reocclusion), as well as reducing cardiovascular disease risk factors to buy you valuable time to make healthy lifestyle changes.
Once you get your risk factors firmly under control (i.e., lose weight, quit smoking, reduce blood sugar), your doctor might decide to reduce or stop some or all of your medications.
*Important! Advise your doctor if you’re taking any dietary supplements, as some of these can interact with your medications and cause serious harm. For example, medicinal mushrooms have many health benefits, but constituents in these products can react with your medications and cause a dangerous drop in blood pressure or blood sugar.
Beta-blockers
Beta-blockers slow down your heart rate which also helps to reduce blood pressure and, consequently, workload on the heart. They also help relax your blood vessels which can improve blood flow and reduce or prevent chest pain (angina).
Blood thinners
Blood thinners like aspirin and Clopidogrel (Plavix) reduce clotting, improve blood flow through narrowed arteries, and reduce your risk of a heart attack.
Nitrates
Nitrates (such as nitroglycerin) are tiny sublingual (under your tongue) tablets which relax and widen your blood vessels to improve blood flow and reduce angina symptoms.
Statins
Statin medications lower your blood cholesterol by blocking precursors needed to synthesise cholesterol. They reduce accumulation of plaque in your arteries and minimise the formation of new blockages.
Calcium channel blockers
Calcium channel blockers relax and widen your blood vessels to increase blood flow through your heart and prevent angina. Some classes of calcium channel blockers (non-dihydropyridine) also reduce heart rate to lower strain on your heart.
ACE inhibitors
Angiotensin Converting Enzyme (ACE) inhibitors block an enzyme that produces angiotensin II, a substance which constricts your blood vessels. Blocking the formation of angiotensin II relaxes your blood vessels and lowers strain on your heart.
Lifestyle changes
Lifestyle changes are a non-negotiable after angioplasty. These include:
- Regular exercise
- Non-exercise background physical activity
- Healthy diet rich in heart-protecting fruits and vegetables
- Stress and anger management
- Behaviour modification to maintain lifestyle changes
Remember that angioplasty is not a “cure-all” for your coronary artery disease. As with medications, angioplasty buys you crucial time to establish lifestyle changes that can massively reduce your risk of having a first heart attack (or a second heart attack if you already had one).
*Important! There are lots of unscrupulous marketers looking to sell you snake oil. Check out Dr Gabrielle Maston’s article on the pros and cons of the Paleo Diet after a heart attack, as well as my consumer advocacy articles to protect you from health scams.
- 37 Bullshit Health Marketing Phrases You Should Ignore
- Want to Be Healthy? Then Stop Chasing Golden Unicorns
- Skinnyfit Detox Review: A Detox From Toxic Marketing
- Interactive Bullshit Detector for Health Products
- Macronutrient percentage calculator
Benefits of exercise
You know exercise is good for you, and there’s solid scientific evidence that says you should exercise soon after an angioplasty and stent.
Here’s a quick list of exercise benefits to get you in the exercise mood:
- Reduced risk of a heart attack (or second heart attack if you’ve already had one)
- Improved heart function (i.e., lower heart rate and blood pressure means less workload on the heart)
- Increased anginal (chest pain) threshold. The more fit you are, the harder you have to work to elicit chest pain (if there are blockages present)
- Improvements in oxygen delivery (via the blood) and consumption (in your muscles)
- Enhanced fuel selection with exercise (i.e., your body can tap into fat easier with better conditioning)
- Body composition improvements (i.e., reduction in fat, particularly dangerous fat around the organs)
- Improved blood sugar control and insulin sensitivity (if you have diabetes)
- Increased functional ability (i.e., easier to perform activities of daily living like lifting boxes, gardening, cleaning the house)
- Increased quality of life
Post-operative exercise risk
Exercise raises your heart rate and blood pressure which also raises your risk of bad things happening to you. Worst case scenario is you could have another heart attack or die.
To put you at ease, if you’ve already had a cardiac event and intervention, then your “volcano” has already erupted. I’m honestly more fearful of exercising the person with all the risk factors who has NOT had an angioplasty because they’re a potential ticking time bomb. Cliche as it sounds, better the devil you know than the one you don’t.
Here’s the good news: with proper screening and taking precautions, you can significantly reduce these risks and reap all the protective benefits exercise has to offer.
Can exercise damage the stent?
It’s uncommon but stents can sometimes fail. Overexerting yourself during the recovery phase can increase this risk and potentially cause problems with your stent. Stick to low-level activities and follow your doctor’s advice.
When can I exercise after angioplasty and stent?
After your surgery, you’ll probably feel great (provided you’ve not had a heart attack or other complications) because your heart muscle is now getting lots of oxygen through the newly reopened arteries.
*Important! Even if you’re feeling awesome, know there is still healing happening on the inside!
For example, I had a client who called me up and wanted to start training on the same day. I had to grab him by the proverbial scruff of the neck and bring him back down to Earth. I was happy he was enthusiastic, but he still had some healing and recovery time ahead of him before we could safely work together.
Initial recovery activity after discharge
Give yourself at least two weeks of low activity recovery time after leaving the hospital. The logic is that while your angioplasty and stent are still fresh and settling in, you want to avoid any sharp increases in heart rate or blood pressure (which strenuous exercise will do).
Go for walks around your neighbourhood on flat terrain, but leave the mountain climbing and pumping iron to Arnold (for now).
You will also need time for your body to adjust to your medications and understand how your body responds to them when exercising.
Pre-exercise planning
If you plan on exercising hard (either aerobic or strength training), talk to your cardiologist about having a treadmill stress test (probably around 4 to 6 weeks after your angioplasty).
This will give you valuable information on how your heart is working after the procedure and recovery phase, and it can inform the types of exercise workloads that your body will safely be able to handle.
If you can tolerate high workloads without any signs or symptoms (ie., chest pain, shortness of breath) or unexpected arrhythmias on the electrocardiogram, then this is pretty good assurance that you’ll be able to push the higher exercise intensities on your own.
Aerobic exercise after angioplasty

Aerobic exercise is safe and effective to help build your cardiac and overall body endurance. Not only does it help the heart muscle itself, but it improves the biochemical efficiency of your entire body and the way it uses oxygen and nutrients to fuel exercise. This means that, as you become fit, you are able to tolerate higher workloads with less overall stress on your heart muscle.
Post-angioplasty exercise plan
After an angioplasty, it’s important that you gradually build up your aerobic fitness. The safest way to do this is through a graduated exercise plan.
I adapted the following sample graduated exercise plan from cardiac rehab to progress you from shorter to longer exercise durations over several weeks. The pattern is that you do short exercise bouts more times per day, and as you progress through your recovery, you add more time and transition down to fewer times per day until you’re able to do long continuous exercise in the 30 to 60 minutes range.
| Week | Minutes | Times Per Day |
|---|---|---|
| 1 | 3-5 | 6-8 |
| 2 | 5-10 | 4-5 |
| 3 | 10-15 | 3-4 |
| 4 | 15-20 | 3 |
| 5 | 25-30 | 2 |
| 6 | 30-45 | 2 |
| 7 | 60 | 1 |
How often can I exercise?
After you’ve cleared the first month of recovery, start off with 3 to 4 days per week and work up from there. If you were active before surgery, you have the advantage of muscle memory and a residual training effect. But it’s still important to “test out” your body during exercise see how your heart rate and blood pressure respond (and the effects of the medications).
How hard can I exercise?
Keep exercise intensity on the lower end to begin with and gradually progress to higher workloads. Start at 50 to 65% of your maximum heart rate and see how you feel. If it’s too light, you can try a different training range of 60 to 75%.

Shop around for fitness tracker watches that meet your needs, from a basic heart rate monitor only to more advanced, whole-body solutions that track your sleep, incidental movement, and calorie expenditure.
If you’re on medications that lower your heart rate, then heart rate calculations will not help. I’ll discuss the talk test and Borg’s rating of perceived exertion below to help you find a safe exercise intensity.
Determining exercise heart rate
If you’re looking for a training target heart rate, then here are two common calculations:
- Straight heart rate method
- Karvonen (heart rate reserve) method
For both methods, I’ll use an example of a 50 year old man with a resting heart rate of 60 bpm.
Method 1: straight heart rate calculation
1) Determine your estimated max heart rate by subtracting your age from 220
- 220 – 50 = 170 bpm estimated max heart rate
*Important! If you have an actual MEASURED max heart rate from a stress test, use that number.
2) Calculate training percentages based on 170 bpm (or your actual measured max)
If you want to exercise at 50 to 65%, calculate as follows:
- 170 x .50 = 85 bpm
- 170 x .65 = 111 bpm
Therefore your training heart rate range would be 85 – 111 bpm.
If this range is too low and you wanted 60 to 75%:
- 170 x .60 = 102 bpm
- 170 x .75 = 128 bpm
Therefore your training heart rate range would be 102 – 128 bpm.
Method 2: Karvonen (heart rate reserve) method
The Karvonen or heart rate reserve method incorporates your resting heart rate.
1) Subtract your age from 220 to get your theoretical max heart rate
- 220 – 50 = 170 bpm
2) Then subtract your resting heart rate
- 170 – 60 = 110 bpm
3) Calculate your training heart rate percentages from this. Let’s say 60 to 75%.
- 110 x .60 = 66 bpm
- 110 x .75 = 83 bpm
4) Add back in your resting heart rate
- 66 + 60 = 126 bpm
- 83 + 60 = 143 bpm
Therefore, your training heart rate range would be 126 to 143 bpm.
Heart rate calculations are not one-size-fits-all. Start at the lower heart rate percentages and adjust accordingly until you find a comfortable starting pace.
Check your pulse on your wrist or carotid artery. If you have difficulty, look into getting an inexpensive heart rate monitor. Smartphones also have this capability now.
Heart rate calculator
I’ve created a super simple heart rate calculator below (because math sucks!). Select which calculator you want to use and then input your age and heart rate for your result.
Simple HR Calculation
Karvonen HR Calculation
The talk test
Some medications can blunt your heart rate (i.e., beta blockers), rendering heart rate calculations reasonably useless. In that case, you’ll need to rely on what’s known as the “talk test.”
You’re looking for a moderate intensity, so if you can have a conversation with someone while exercising and you’re not gasping for air, then this intensity should be sufficient. But you also need to feel like you’re doing some work because you don’t want it to be too easy.
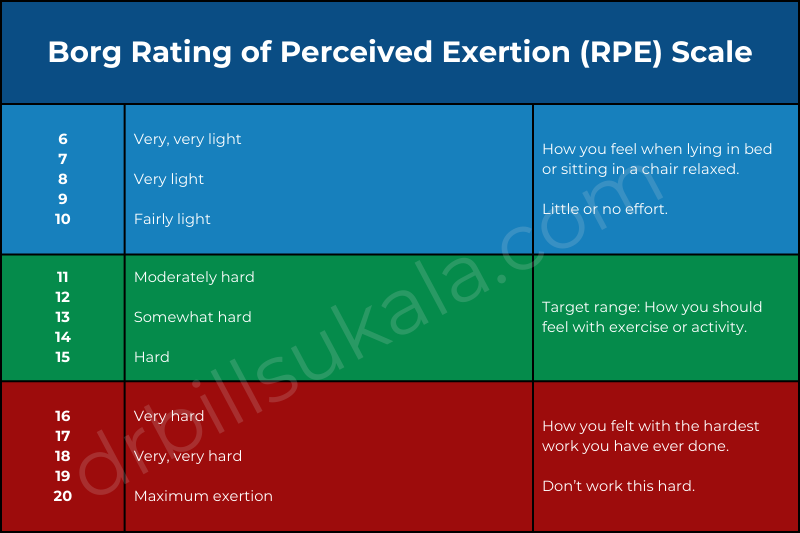
Rating of perceived exertion (RPE)
The Borg rating of perceived exertion (RPE) is a 6 to 20 point scale for assessing exercise intensity. The logic behind a 6 to 20 scale is that most people at rest or doing light activity have a heart rate between 60 to 90 bpm. If you’re working very hard, then you’re going to be around 170 to 200.
Borg then decided to just drop the zeros and create a scale which is consistent with most heart rates at a given workload.
This is particularly useful if you’re taking medications that slow your heart rate. There is a bit of a learning curve to it, so if you go to cardiac rehab, the staff can give you a first-hand demonstration.
How many minutes of aerobic exercise?
Start off with 10-20 minute bouts of exercise and assess how you feel immediately after and the following day. If you feel drained, you may need to scale it back. Otherwise, you may wish to increase the duration.
If you need to do several small intervals to accumulate your daily exercise minutes, then break them down into small intervals you can comfortably tolerate. For example, walk 10 minutes, take a break, walk another 10 minutes, take a break, and then a final 10 minutes for an accumulated 30 minutes total exercise time.
Which types of aerobic exercise are best?
Aerobic exercises that are rhythmic and continuous and incorporate the large musculature of your body (i.e., hips and legs) will give you the most exercise bang for your buck. This includes walking, jogging, running, bike riding, swimming, or trail walking around your neighbourhood. Ultimately it’s important to pick exercises you enjoy since this will help you stick with it.
Aerobic exercise precautions
- Clearance: Make sure you’re safe to exercise. Get your doctor’s clearance to exercise first.
- Warm up: Always warm up with light activity to dilate your blood vessels and prepare your body for lifting (and minimise risk of a spike in HR and BP).
- Progress slowly: Keep it simple and progress slowly over time. Doing too much too soon can potentially lead to complications.
- Flat terrain first: Stick to level terrain in the early stages and as you progress through recovery, you can slowly include hills or other inclines.
- Environmental stressors: Limit your exposure to extreme heat, cold, wind, or other stressors, particularly in the early stages of recovery, as these will place additional stress on your heart.
- Adverse events: Continually monitor yourself for any strange symptoms either at rest or during exercise, such as chest pain, tightness, arm or jaw pain, pain between the shoulder blades, shortness of breath, or dizziness. Contact your doctor immediately if you experience any of these.
Lifting weights after angioplasty

Can you lift weights after angioplasty? Absolutely.
In fact, according to a 2023 Scientific Statement by the American Heart Association, not only can resistance training improve or maintain muscle mass and strength, but it has many beneficial clinical effects on cardiovascular disease and risk factors, including:
- Lower blood pressure
- Better blood sugar control
- Lower lipids (cholesterol, triglycerides)
- Improved body composition (fat vs muscle) and body weight
- Reduced arterial stiffness
- Reduced inflammation
- Increased fibrinolysis
- Improved endothelial functions
- Lower depression and anxiety
- Better sleep
- Improved quality of life
Considerations before you lift weights
Getting into weight lifting depends on a number of factors that should be carefully discussed with your medical management team:
- Did you have a heart attack?
- Was there any damage to your heart muscle?
- Do you have any arrhythmias stemming from the heart attack?
- Do you have high blood pressure?
- Are you taking medications to lower your heart rate and blood pressure?
- During the cardiac catheterisation, did they note how widespread the coronary artery disease was (i.e., one artery, two arteries, triple vessel disease)?
- Did they stent all the offending arteries or were there still arteries with lower levels of plaque they chose not to stent?
- Were you a regular weight lifter before your procedure?
- How much weight were you lifting?
If you had damage to your heart muscle or have arrhythmias and high blood pressure then high intensity weight lifting might be contraindicated (not advised) until you’re medically stable.
If you have other arteries with blockages that are being medically managed, these plaques could theoretically rupture with heavy weight lifting.
If you were a weight lifter before your angioplasty, then you might have a greater tolerance for higher loads and better technique to lift safely.
How often can I lift weights after the procedure?
Start with a frequency of twice per week and gradually work up to 3 – 4 days per week as tolerated. Similar to aerobic exercise, you will want to ease into it and monitor yourself for any signs or symptoms, including spikes in heart rate or blood pressure.
How much weight can I lift?
It depends. You’ll need to work closely with your medical management team (including cardiac rehab staff) to determine a appropriate starting weights that do not elicit any dangerous changes in heart rate and blood pressure, or other symptoms like dizziness or shortness of breath.
Increase your weights in small increments of approximately 5% per week as appropriate. The increases will likely be smaller with the smaller muscle groups like arms and shoulders and a bit larger for bigger muscle groups like the legs and hips. Do not go up in weight if you’re still struggling with your existing program.
Can I lift heavy weights?
If you’re into bodybuilding, Cross-Fit, or Olympic lifting, you’ll need to weight out risks vs rewards. You need to first establish a strength training foundation with lower weights (with no signs or symptoms).
You will also want to do a treadmill stress test with your cardiologist to ensure that your heart is still strong and stable at high workloads. If all this is in order, your doctor may clear you to progress to the big weights.
How long should my weight lifting sessions be?
There’s no firm answer to this since it depends on how many exercises you do and how many sets and reps of each exercise. Go by trial and error and see how you feel the following day. If you feel depleted and run down, you might want to do fewer sets to lower the duration. As your fitness increases, a longer training duration will be better tolerated.
What types of resistance exercise is best?
Resistance training comes in all shapes and sizes. Check out these examples, including adjustable barbells, dumbbells, cables, kettlebells, set of TRX straps, or even good old fashioned body weight exercises like push-ups and chin-ups.
Resistance exercise precautions
Resistance exercise is recommended after an angioplasty, but heed these warnings to reduce risk and ensure your safety:
- Clearance: Like with aerobic exercise, get your cardiologist’s approval to exercise.
- Foundations first: First build a solid aerobic fitness base. Some of these fitness gains will help you safely transition to weight training and tolerate higher loads.
- Progress carefully: Gradually work up to heavier weights and higher training volumes.
- Warm-ups: Always warm up on the bike or treadmill to dilate your blood vessels and prepare your body for lifting (and minimise risk of a spike in HR and BP).
- Environmental considerations: Be careful lifting in very hot or cold climates. These are additional stressors that can put more strain on your heart. Try to exercise in climate controlled conditions.
- Adverse events: Continually monitor yourself for any strange symptoms either at rest or during exercise, such as chest pain, tightness, arm or jaw pain, pain between the shoulder blades, shortness of breath, or dizziness. Contact your doctor immediately if you experience any of these.
Stretching and flexibility training
Stretching and flexibility training is great exercise after an angioplasty. You might be tight and stiff after being stuck in a hospital bed and recovering at home, so range of motion exercises will counteract this.
If you’re doing aerobic and strength training, stretching will reduce muscle tightness, improve mobility around your joints, and reduce your risk of injury. Overall, you will feel more limber and relaxed in your daily living.
Stretch your major muscle groups, including your large muscle groups like your hips, legs, and mid-section (back, abs, obliques), and your smaller muscle groups like your arms and shoulders. If you’re exercising at home and not sure where to begin, there are numerous stretching books on the market to get you started.
Stretch within your pain-free range of motion. As you feel the pull on your muscle, work to a point where it’s mildly uncomfortable but NOT painful. If you say “OUCH” then you’ve gone too far. Remember that you must build flexibility slowly over time.
Playing sports after angioplasty
You can play sports after angioplasty but, depending on your sport, you must discuss the specifics with your cardiologist. If you play contact sports like football, hockey, or boxing and you are on blood thinners, blows to the body can cause internal bleeding. These might not be advisable until your doctor reduces or takes you off the meds.
For high intensity explosive sports like basketball, tennis, or the latest craze pickleball, make sure you have a solid aerobic fitness foundation first (likely 1 to 2 months after your angioplasty) and clearance from your doctor.
Low intensity sports like golf, swimming, or light dancing are probably safe after the recovery period. However, the explosive movement of swinging a golf club too soon after your procedure might not be approved by your doc until you’ve been to your follow-up appointment and received the all clear.
Take home message
The bottom line: there is life after angioplasty! You CAN exercise safely if you stick to science and work closely with your medical management team.
No matter if you prefer cardio, lifting weights, or playing sports, speak with your cardiologist about your medical and exercise history to determine the best approach. Ask lots of questions and don’t give up until you have the answers you’re seeking.
I highly recommend cardiac rehab because this will provide a safe environment with knowledgeable staff to help you exercise safely and monitor your vital signs. The nurses and exercise physiologists and/or physical therapists are an extra set of eyes and ears and a rich source of information to help you feel more comfortable exercising.
Once you adapt to the changes, there’s no reason why you can’t live a healthy and active lifestyle again.
Check out related links on this site for exercise after:
Dear Dr Bill Sukala, thank you for your excellent and informative article. I recently had a 2nd stent fitted inside the original stent (70-80% blocked) in the LAD, because the 1st one developed excessive cellular growth over the stent (became 90% blocked with cells). I am a keen cyclist and resumed normal-strenuous riding after getting the clearance from my cardiologist about 6 weeks after my 1st stent (drug eluting). Have been on several typical medications after stent placement. I have been trying to find evidence that strenuous cycling after a stent may induce excessive cellular growth in a stent and may explain my situation. Would be interested in your thoughts. thanks Joe
Hi Joe,
Thank you very much for taking the time to leave a comment. I am aware of this occurring in some cases, but I do not know the extent to which cycling would contribute to or hasten its development. Have you had a heart attack at any point or was it just coronary artery disease followed by angioplasty/stent? If you’ve not had a heart attack (and no resulting myocardial damage), then you’re mainly dealing with a “plumbing job”rather than a “heart job.” So this at least puts you in a better position. Have you had any follow up on the second stent? I think in your case you’d be well advised to pay special attention to any signs or symptoms which might be indicative of any subsequent blockage. Regarding in-stent stenosis, have a look at these articles which might provide a bit of scope and insight into why this happens: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767562 and https://www.ncbi.nlm.nih.gov/pubmed/9697822 and https://www.ahajournals.org/doi/full/10.1161/circinterventions.110.957332 Feel free to keep in touch and drop me a line if you find out anything. It is indeed an interesting situation and you are not alone in this happening. Kind regards, Bill
Josephy and Dr Sukala, I had the exact same situation with myself, at the age of 42 I had a full on heart attack, stopped breathing for 15 minutes…luckily my friend was there and knew CRP and she kept me going until the police arrived with a defib’. But fast forward by 2 years to December 2018 and the stent that was placed became 99% blocked, so same remedy I had another stent placed inside the old one.
None of the specialists I’m dealing with seem to be able to answer why this happened. I had totally changed my life around and was at the height of fitness running 15km twice a week and doing regular boxing bootcamp (non contact) ….Is there any chance i can compare notes with you Joe?
I would be grateful.
Respected Dr. Bill
Would like to have your advice regarding start of Swimming after Angioplasty. Lvef is 55-60%, with no RWMA, 3 stents placed after atypical Angina in OM terminal, OM1/and LAD proximal with 50% stenosis in RCA. I would be pleased if u can give me ur email ID where I can send u the discharge summary and Angioplasty report for proper opinion.
Thanks Dr. Jyotsna Verma
Liver Transplant Consultant
Hi Dr Jyotsna,
Thanks for leaving a comment. You can send me an email by visiting my contact page on this website. There you will find my email address. Kind regards, Bill
Hi Bill,
I had a heart attack at the beginning of November, I has a stent to my LAD. although
there was atheroma, it was diffuse and my cardiologist said for my age (45) that it
wasn’t abnormal. What was abnormal was the size of my arteries, mostly they were
very large apart from one place where they were naturally much smaller, (where they
placed the stent).
The heart attack came directly after a very intensive session with a personal
trainer. I’ve been going about three months and being quite a competitive person I’d
enjoyed being challenged by the PT to push myself as hard as possible. In my younger
days I’d climbed mountains, sailed and biked, i was very active. In my later 30s
work took over and I put on a far bit of weight, the PT was a way of fitting
exercise into my life.
Since then I’ve changed my life a lot, I’ve moved countries, from the UK to Spain,
changed jobs. I walk every day for sixty minutes.
My issue is weight loss and other exercise, my thoughts go from feeling like there’s
nothing wrong with me to real anxiety that if I don’t do something that I will die
an early death. I’m afraid of doing any exercise that significantly increases my
heart rate, I feel paralysed by this… I’m stuck!
Stew
Hi Stew,
Thanks for your message. Just to reassure you, it is quite common to experience anxiety after a heart attack. Clearly you want to be out doing healthy things, but it’s always in the back of your mind that it could happen again.
First, remember to deal with what IS rather than worry about something that hasn’t happened yet. If your doctor told you that your other arteries are clear and that your stent in the LAD is completely patent with no restenosis,then that is a good sign.
Second, you also have to remember that most people who have heart problems usually have symptoms and, if you pay attention to them and get treatment, then you should be fine. It’s people who ignore signs and symptoms (i.e., crushing chest pain) that end up in the morgue.
Third, exercise is supposed to cause your heart rate to rise, but you do have control over the intensity. If you’ve done a stress test with your cardiologist and he/she told you that you have a ticker the size of a thoroughbred racehorse with no abnormalities on the ECG, then that is good assurance as well.
Fourth, I would also advise speaking to a counsellor with experience in helping people with medical issues. This is a sign of strength and not weakness. You clearly want to do the right thing by your health, but if you are physically well as confirmed by your cardiologist, then it may be time to get back on the horse. If a counsellor can help you work through a few sticking points, then perhaps that can get you back on the straight and narrow. It’s ok to be human. I have worked with a LOT of people over the years with medical issues and, if you’re getting back into your activity in a systematic way and ticking all the safety boxes, then you can say with reasonable confidence that you’ll be ok. But again, I want to emphasise that there’s no foul in speaking to a counsellor to work through any sticking points you might have.
Feel free to leave me a comment or any other questions you might have. Happy to help where I can. Kind regards, Bill
Thanks Bill, it took a few days for me to really process your response, I think part of the problem is that I wanted a “big bang” and that maybe I was also being paralysed by that. I think I need to make small changes more often rather than head for a long day in the hills or do a 50k day on my bike, that should reduce anxiety from not doing anything and the anxiety that i’d over exert myself
Thanks for your help
Greatly appreciate the exercise guidelines, precautions and contraindications. I am a personal trainer who just took on a client who recently got 3 stents put in. Confident I can now design a safe but challenging and effective workout regimen to get him back moving again.
Hi Dorian,
Thank you for taking the time to leave a comment. As a trainer, you know the exercises but the real magic in training your cardiac clients is in knowing the signs/symptoms of when something’s wrong. In all honesty, if your client has been cleared by the cardiologist or, even better, has had a successful run through a cardiac rehab program, then you should be fine. Keep an eye on the heart rate and blood pressure, as well as understanding the impact of your client’s medications on the exercise response. How long has it been since the stents were placed? Happy to help if you have any other questions. Kind regards, Bill
3 stents were placed 2 months ago, I just met the client and before anything, I asked for a doctor’s clearance
Excellent. If he’s two months post-stent, then that’s plenty of recovery time. Good move getting the doc’s clearance as well! Best wishes to you both! Cheers, Bill
Hi Dr I had a stent operation two months ago and up until now I still feel weak. I’m 60 years old and the daily medication I have now is Effient 10mg, Triatec 2.5mg, Salospir 10mg and Liptruzet 40mg. I did have my follow-up check up and my doctor says all is running smoothly. My worry is that I still feel very weak although I do some excercise/working every day for about 40 – 60 minutes. Pls your comments. Thanks
Hi Elias, I’m sorry to hear that you’re feeling weak. It’s difficult to say exactly why this might be, but would certainly be worthwhile speaking to your doctor about this. Looking at the medications you’ve listed, you are taking a platelet inhibitor (Effient), ACE inhibitor (Triatec), aspirin (Salospir), and a cholesterol med (Liptruzet). I don’t think the first three medications are unlikely to cause this side effect, but doing a bit of digging, the Liptruzet, as with any other statin medication, could plausibly cause your muscle weakness. Common side effects of Liptruzet include nausea, muscle pain, tenderness, weakness, increased fatigue, and dizziness (among others). Bottom line: it would be a good idea to speak with your doctor about this regarding the cause of your weakness and the possibility that it could be a side effect from your statin medication. Hope this helps. Kind regards, Bill
Hi Bill, thanks for the article. I’m 56 and had a PTCA/Stent thing done almost 4 months ago here in Perth. I’m lucky that I had the opportunity to attend a rehab education class and a free 16 session rehab gym program at the hospital (thanks Fiona Stanley!). The thing that made a big impression on me was the “talk test” you mention. I’m on a raft of various pills, so it’s difficult to work out a true indicator of resting heart rate etc – but, I really took to the talk test after our exercise physio said to use it (at our education sessions). I’m a mad keen squash player and I set myself my personal goal of resuming squash after my “compulsory” 6 week period on the bench (my GP was very strict and brooked no argument!!). So, I started the gym sessions and then squash – AND I always kept the talk rule: if I couldn’t hold a conversation while working out, then I was risking a problem. So, maybe I didn’t startle anyone with my squash skills for a couple of months (after the 6 weeks), But I was playing, and I took it really easy. It helps if your squash mates are careful for you too! Now, I’m back to nearly full tilt on the squash court – I’m a terror for three 45 minute sessions a week! I’m even winning some games!! But, truthfully, I still monitor my progress, and I often just take a moment to re-gain my breath between serves. There’s no shame in being careful. I’ve got nothing to prove to anyone at my age.
As for the gym, that’s been twice a week. It’s just finished at the hospital, and I’ve joined a 24-hour joint just down the road. I’ve never been to a gym before, but I’m enjoying that too. For those of us that get bored with long sessions on walking machines etc, I recommend an MP3 player/iPod or equivalent, loaded with podcasts or music or audio books. It’s amazing how easy it is to get through the boredom when your distracted by a good book!!
Thanks
Hi Michael, I very much enjoyed reading your comment. You are a perfect example of someone who didn’t just throw in the towel and accept life was over after this little heart plumbing incident. Provided you did not have a heart attack and did not have any heart damage, not to mention an uncomplicated angioplasty/stent procedure, you’re clearly in a good place to heal up well and get back to living life to the nines. I also enjoyed that you bit the bullet and heeded the precautions during your recovery. I’ve seen people push it a little bit too hard during recovery and end up with a collapsed stent, although will admit this isn’t a common occurrence. I like that you’re back playing squash as well. I used to be a pretty hardcore racquetball player back in the US and I can see that, although the sports are different, they’re both pretty strenuous. Well done on an excellent recovery! Big fan of your work! Cheers, Bill
Dr. Bill,
I have been reading information you have provided on heart attacks/problems.
In particular the advice you gave Michael a 56 man from uk.
I had a coronary heart attack on the 18 Nov 15, I basically ignored signs like pins & needles plus a heavy indigestion for 3 days.
The medical services were great I had a stent put into the coronary artery, the angioplasty check up was perfect no bruising or damage whatsoever.
I’m now attending the cardio physio team twice weekly.
Like Michael I’m a keen squash player, thinking of playing again if safe but the cardio physios aren’t that keen on it because the BP & pulse goes through the roof they say.
Normally my pulse playing squash & when running on the treadmill works upto 190ish , they are recommending about 90’s pulse, this might be too boring for me squashing. I noted your advice for Michael questioned whether he had a heart attack.
Also mentioned was a stent could be damaged.
I’m taking advice from the team so I will wait & see. Also thinking of using light weights..
Hi Tom,
Thanks for your comment. First and foremost, remember that you’re pretty fresh from the heart attack and angioplasty/stent. Even if you feel great after your procedure (which is great), there is still healing happening on the inside. At this early stage, you do need to be careful and give your heart some time to recover. I will admit, I’m also a bad patient when it comes to injuries and I have a hard time not being active as well, so I can empathise with your situation.
The questions that are important to consider here are:
1) Did you have any damage to your heart muscle?
2) Did they give you any indicator of how much damage? Any idea on an ejection fraction?
If you’re working with a cardiac rehab them, then this is a very smart move on your part. They will be familiar with your particular medical history and surgical reports. Discuss those questions with them when you next see them.
Also, if you’re on medications such as a beta-blocker, then this will reduce your heart rate a fair bit and “save you from yourself.” I’m not a fan of medications, but there are times where they can be beneficial particularly in the recovery phase after a heart attack/surgery in order to keep down the heart rate and blood pressure.
Best wishes and feel free to report back here with an update so others may benefit.
Kind regards,
Bill
@Michael, Thank you. Your perspective was extremely useful. I too had a “plumbing” incident versus a heart attack and patience is not one of my strong suits. I was feeling great and ready to return to my previous regiment. So reading about how you “bit the bullet” and followed instructions with your recovery was very motivational. Your report on the benefit long term for following instructions was also very encouraging.
Dear Dr Bill
thank you for the article on exercising after an angioplasty, it has put me in a positive frame of mind.
I am a 55 year old British man, working as a teacher in Taipei, Taiwan. I do not smoke, I eat sensibly and enjoy beer within government-recommended guidelines, I swim, cycle, and walk at least three times a week, and my BMI is around 23. My maternal grandfather died of a heart attack in his 50s, but my 80 year old father is as strong as an ox.
About two months ago at the end of August 2015, I went to hospital feeling tired and breathless, and was rushed to the emergency room where I was diagnosed with unstable angina. I had to remain in the hospital for five days. This came as a a tremendous shock to me because the week before I started to feel unwell, I had been exercising as normal. Now I am waiting for an angiogram sometime in December. In the meantime I find I can walk steadily for about an hour, and I can do qi gong, but anything more leaves me breathless.
I feel very frustrated because I obviously want to educate myself about atherosclerosis, but every time I get on the net to check it out, I read that I should ‘lose weight…’, ‘stop smoking…’ etc. etc. none of which applies to me.
Something I should add is that for the past year I have been waking up at night with myoclonic jerks. This is a complete nightmare and I wake up most mornings feeling exhausted. I had a sleep study and was diagnosed with sleep apnea [in which you stop breathing in your sleep]. I am renting a CPAP [a kind of air pump and mask] for the time being, and the data from the pump tells me that I have central sleep apnea, that is to say the brain is not instructing the lungs to breath.
The medical professionals I am dealing with here are all Chinese speakers but most of them speak English to a greater or lesser extent [far better than my Chinese…], and they are doing their best for me. However, there is an inevitable language barrier and comprehension gap.
My question to you is this: is my atheroslerosis caused by my sleep apnea, or is my sleep apnea caused by my atherosclerosis? Furthermore, if I have a stent implanted will I be able to send the pump back to the distributor and get a decent night’s sleep again?
Thank you in advance, best wishes, Dave
Hi Dave,
Thank you for taking the time to write such a thoughtful and detailed comment. With regards to your questions, there is evidence that sleep apnea is associated with atherosclerosis in individuals without any other significant risk factors.
Regarding your second question, I’m not under the impression an angioplasty/stent will “cure” the sleep apnea, so your best bet it to speak with your doc about your treatment options for the apnea.
Have you considered heading back to the UK for treatment (even if only temporary)? Perhaps find a specialist centre that deals with a lot of sleep apnea cases and get top notch treatment. Alternatively, since you’re obviously part of the commonwealth, perhaps a trip to Australia for treatment since it’s not too far away?
Keep us posted on how you go, Dave.
Kind regards
Bill
Dear Dr Bill, I am 48 and I was training for my first Ironman, (I´ve done several triatlones, couple of 70.3, lot´s of 1/2 marathons and three marathons) when I started feeling tire with pain in the chest and arms, I stopped and got my self checked, the result was 3 stents.
At the beginning I was psicological destroy, and the first feedback was that I could´nt run marathons again needer 70.3… not to think on an Ironman, that hit me hard!!!, I am going to get a doble opinion but I would love to hear your thoughts. I just started after one month from the intervention to swim, ride the bike and run again, keeping good look at my heart rats and for periods not longer that1 hour. I would love to run a couple more marathon, I feel that without the challange of long distance races I would stop doing this….
Look foward to your thoughts…
Cheers
Muy buenos dias Carlos, Perdon la demora en contestarte pero estoy viajando al extranjero (de negocios) y no he tenido tiempo para responder bien. En cuanto a tu situación, legalmente no te puedo dar consejos específicos porque no se todos los detalles de tu condición.
Primero que nada, recomiendo que hables con tu cardiólogo y si tu condición esta estable, preguntale si puedes volver a tu entrenamiento. O buscale a un cardiólogo que haga ejercicio (o tenga especialización en medicina de deportes) que realmente entienda tu pasión por ejercicio y deporte. Seguro te hicieron un angiograma. Visualizaron tus otras arterias para asegurar que no hay obstrucciónes en ellas?
Segundo, a ver si te pueden hacer una prueba del esfuerzo cardíaco. Si no hay irregularidades en tu ritmo cardiaco o el segmento ST en el electrocardiograma seria una buena indicación (echale un ojazo a esta pagina: http://www.my-ekg.com/como-leer-ekg/segmento-st.html).
Tercero, si no tuviste un infarto y no hay daño al músculo cardiaco, significa que tuviste un problema de pipas tapadas y no del corazón.
Quarto, de aqui en adelante, lo mas importante es estar atento a tus sintomas. Los sintomas que tuviste son relativamente comunes y si los tienes de nuevo, sabras que tienes que ir al hospital. Es importante no esperar porque “tiempo es músculo cardiaco.” Una arteria tapada, sin tratamiento, puede causar daño al músculo del muro cardiaco.
He trabajado con pacientes cardiacos que hacen mucho ejercicio y con tiempo lograron volver a entrenar y competir. Es posible pero lo mas importante es mantener la comunicación con tu cardiólogo y respetar a los síntomas.
Gracias por dejar un comentario y espero que esta info te ayude.
Cheers,
Bill
PD, vivia en Mexico por eso te repondi en español.
Orale Guey…..Extraodinario!!!
estoy siguiendo tus recomendaciones exactamente, fui a un cardiologo de deportes, y me pidio un test de esfuerzo con MiBi??, en fin me lo hago en un par de dias.
lo mio fue afortunadamente un episodio que no llego a ser infarto … solo de cañerias.
y el resto de las arterias estaban normal.. me dejaron con aspirina, brilinta, nevilet, crestol, omeprazol…
ya estoy corriendo, nadando y pedaleando nuevamente manteniendo las pulsaciones en 135…
asi que muchas gracias por responder!!!!
saludos.
Sipo huevon! Jaja, buenas noticias! Creo que con esa información te dará más paz interior sabiendo que todo está bien. Me parece un buen cardiólogo también. En tu caso, creo que necesitas alguien que entienda la mentalidad de un atleta. Suerte matador! Manda notícias cuando tengas la medalla de oro en la mano!
Any chance you can put this one in English?
What language was it?
Dr Bill thanks alot for your useful information
My brother in law is 53 year old last week he went in to stent angioplasty but he had sugar as doctor said his gear is very weak need to some simple exercise ..am confused how he should reduce sugar level and be healthy
Hi Vidyashree
If I understand your question correctly, it sounds like your brother in law has diabetes or perhaps pre-diabetes (with elevated blood glucose). I’d recommend that he seek a consultation with a clinical dietitian in your area for a proper evaluation and consultation to help him better manage his blood sugar levels. And yes, exercise is also going to be an important addition to help reduce his blood sugar levels as well. Ask your doctor for a referral to a cardiac rehabilitation program as well. This will be a safe way forward to get the best and safest information for your brother in law. Kind regards, Bill
Dr. Bill,
I had 5 stents put in to open 3 blocked arteries 8 weeks ago. Taking statin, Plavix, aspirin & beta blocker.
I’m 50, triatlete, ultra runner, personal trainer and ice hockey player.
Prior to my mild heart attack, my max HB was 185. I have been animal and dairy free since (almost no oils), following Esseltyn/Cambell diet and program. My total cholesterol is now 103 (179 before), LDL 53 (120 before) and HDL still in 30s.
I am back to almost all of my previous activities (teaching Spin, aquavit, jogging, swimming), along with cardiac rehab with no problems at all (keeping hr below 140). My resting hb was below 60 before, and now is a bit lower. I’d like to go back to ice hockey, which is the only activity that raises my hb to around 160-170 in short bursts followed by recovery. I’d like to eventually be drug free, if diet keeps my #s low.
Your thoughts on returning to ice hockey and necessity for drugs?
Thanks,
Leigh
Hi Leigh,
Thanks for stopping by to leave a comment. At 8 weeks post heart attack and intervention, I’d say you appear to be doing very well. I can’t provide any detailed recommendations without knowing your entire medical history, but the things I would suggest speaking to your cardiologist about would be the risk of contact sports (I.e., hockey) while taking blood thinning meds. I’ll be the first to admit that while I’m not an advocate of pumping people full of meds, I think immediately post op they can be helpful to keep heart rate and blood pressure under control during the healing process. Speak to your doctor about your particular condition and if you can safely whittle down the dosages over time. You are clearly health conscious and this will certainly help your case. feel free to stop by and leave a follow up comment to let readers know how you’ve progressed. Cheers, Bill
Hi Dr. Bill, I am 53 year old male. I had a heart attack on 27th of March 2019 and underwent angiogram and angioplasty. The Cardiologist who attended on me has placed a stent in one RPDA and has opened the other with baloon. I have been discharged after three days of the procedure.
Now the doctor has advised me 15 days of rest. I have started slow walking inside my house since two days. I walk almost every hour for 10 to 15 minutes and feel okay. But sometimes feel dizzy and cannot bend as I feel light headed. How much time will it take for me to completely recover? Also I would like to know whether I cam resume my walking, which I used to do before the attack and also push ups after a month or so?
Hi Mohan,
You’re still pretty fresh out of your heart attack and angioplasty/stent. You need to remember that you’re still in the recovery phase and this takes time. You might also be on a number of meds which are commonly prescribed after a heart attack and angioplasty (like beta blockers). Most people start to feel better after a month or so. You said you had a heart attack so depending on how much damage there was to the heart muscle, this can impact your recovery time. The best thing is to have a good long conversation with your doctor about your specific situation to find out what’s an expected recovery time.
You’ll probably have another appointment with your doc in about a month’s time. You should ask about getting approval to resume your usual activity habits. Chances are, you’ll be just fine, but it’s always best to work closely with your doc.
Kind regards,
Bill
Dear Dr. Bill,
Thanks a lot for your detailed information. Yes, my Cardiologist did tell me that I have had some damage to my heart muscle. However, he did not speak in detail as he was busy with some other patients. But as a thumb rule, he told me that I have to take 15 days of rest and can drive only after that.
My Cardiologist has asked me to meet him after a month for reassessment. However, he has told me that I can resume my deskjob after a week. But I am not going to work till the completion of 15 days.
Presently I am taking six different tablets like Clopidogrel bisulphate, Metoprolol Succinate, Ramipril, Pantoprazole, Atrovastatin and Aspirin.
Thanks a tonne once again for your detailed information. God Bless
Hi Mohan
I’m very happy to hear that you’re on top of things. It’s good to be proactive and take an interest in your health. Keep me posted. Feel free to come back and leave another comment to let others know of your progress. I like for these comments to be a resource for others. Kind regards, Bill
Hi,
My name is Janine. My husband Mark had a major heart attack 3 weeks ago aged 55.
For the 30 years we have been together he has been a health and fitness nut.
He’s heart attack occurred after a workout. The main lower artery was 100% blocked.
They were able to clear and put a stent in(thank god) and I do every day). He’s workouts were weight training running martial arts ( kickboxing) . He has mild to moderate damage to the front wall of his heart. My biggest concerns are- he was a man who rarely swallowed a panadol and now he is on 8 different medications inc beta blockers etc.
– his workouts and fitness are part of his everyday life. I’m trying to get a handle on what will be best for him moving forward. Would you recommend an exercise bike or Pilates machine.
His gym equipment consists of treadmill and weight machines .- Dumbbells free weights(long bar one not sure the correct name for that) I just want to see him happy and healthy and do whatever is best. He starts rehab next week. I would appreciate any advice.
Kind regards
Janine.
Hi Janine,
Thanks for your comment. I can certainly appreciate your concern for your husband. He’s not unique in the sense that, yes, whilst exercise is important, it’s not a fix all that protects against all heart attacks. I’ve seen plenty of athletes show up at cardiac rehab with a heart attack and angioplasty/stent. In those cases, there might be a strong enough genetic link that can contribute to it. Thing is, had your husband NOT exercised, it’s also very possible his heart attack would have been much earlier.
I’m glad to hear he’s going to attend cardiac rehab. THAT is a very smart choice. He will have an opportunity to exercise and push himself in a safe environment. Given his cocktail of meds he’s now on, he will need to be aware of both his heart rate and blood pressure response to exercise (and after). Meds that lower his HR and BP both at rest and exercise can sometimes lead to a significant drop in blood pressure after exercise, so tell him to be aware of “post-exercise hypotension.” He can discuss this with his cardiac rehab team.
As for which exercise is best, he’ll need to find exercises that he likes and then test them out under the watchful eye of the cardiac rehab team. Based on your IP address, it appears you’re in Australia as well (Victoria?). Which hospital will he be attending?
Provided your husband is diligent in watching for any adverse signs and symptoms, and if any symptoms do present, then he’d be wise to make sure he gets himself in for treatment asap. I think it’s important to remember that an angioplasty/stent procedure is NOT a cure, nor is open heart surgery. But with very strong lifestyle changes he can significantly minimise his risk of any future events. To be clear, I’m not saying he will have any future issues, but it is something to be vigilant of. As for meds, I admit, I’m not a fan of prescription meds, but when it comes to heart attacks and surgery, they can be helpful for protecting the heart against spikes in heart rate and blood pressure. Down the road, he can speak with his doctor about whittling down the doses as is appropriate.
Hope this helps. Feel free to report back and leave a comment about how he’s going with his exercise regimen.
Warm regards,
Bill
Hi Bill.
Thank you so much for your prompt reply.
You asked which hospital he would be attending.
Initial attack and 000 call we ended up at Jesse McPherson at Monash in Clayton. He had the heart attack late Monday night. He was released on Saturday. Myself I wasn’t happy. They had spent 36 hours draining fluid only to end up giving him a drip on the Friday night due to nausea. He was very pasty looking. When he came home we kept fluids up due to the nausea as they said he was probably dehydrated. Sunday he started with a cough and had a lot of trouble talking without being breathless. By late Monday evening he was getting worse(. I had had him at his GP late Monday arvo) who had given us ventolin. By 1am tues I called 000. He ended up with fluid around the heart and in his lungs and paramedics said he was having minor heart failure. This time he was rushed to Dandenong Valley Private. He has made the decision to stick with them as he found the cardiologist much easier to talk to and felt he was more thorough. (Dr Fernando) it is also closer to home. Myself I’m just scared this will happen again. It is definitely a life changing experience. In a way I’m lucky. My father died from a fatal heart attack at home , so when Mark told me he had severe chest pain I knew not to hesitate in calling 000.
Your reply was very informative and his given Mark a lot to think about. He has always treat his body like a temple so had he not been so fit maybe it would of happened earlier.
Thank you again. Your knowledge has been an immense help.
Kind regards
Janine
Thanks Janine,
This is serious stuff, that’s for sure. Glad to hear he’s being well cared for and appears to be moving in the right direction. Bedside manner is important when it comes to getting a good doctor. There are lots of great doctors out there who are very competent in everything except people skills. Unfortunately, the people skills side of things isn’t a main topic at medical school! Feel free to drop me a line here in the comments section as Mark progresses through his recovery.
Warm regards,
Bill
Hi Bill
Very informative article, thank you.
I have had diagnosed artery disease for about 14 yrs and had a number of procedures to keep me well.
I have two questions :
With a large number of stents can the fact that they are there cause discomfort during cardio exercise ?
At what time do we call a halt to stenting in favour of a bypass ?
Regards
John G.
Hi John,
My sincere apologies for the delay in responding to your questions, but I somehow missed your comment and am only just seeing it now!
For the most part, I don’t believe the stents should cause any discomfort for you during exercise. It’s not to say that it’s not remotely possible, but I’ve never heard a patient say they could feel the stents in their arteries.
As for whether you should stop stenting in favour of bypass surgery, this is generally determined by the surgeon and cardiologist. If you have diffuse coronary artery disease (i.e., lots of blockages) and those blockages are in locations that are critically located (i.e., near a bend in the artery) or they deem the plaque too hard to safely penetrate, then bypass surgery may, in fact, be a viable alternative. Whilst I’m not necessarily in favour of opening anyone up, there are times where it’s the most feasible option to effectively reestablish blood flow.
Hope this helps.
Kind regards,
Bill
Hi, Doctor Bill,
Thank you for this excellent detailed article.
I had my first attack in 2008 while watching a movie at home and one stent was placed. The attack came in March 2015 when I was sailing few miles away from shore on a small boat. The doctor said my first stent blocked 90 % and another artery blocked 75 to 80 %. Hence, first stent was inserted to open the earlier stent, second was placed next to this stent and third stent was used to open the second artery block.
Since then my doctor says I am fine. Kindly guide me, if I can use a bicycle on a plain road (no hills) for small distances (3 to 4 KM) daily?
Best regards,
Sudhir
India.
Hi Sudhir,
Thank you for your comment. Your situation is not unique and I have seen this sort of thing before. It is frustrating, but the most important thing is to be aware of your signs and symptoms and get medical treatment as soon as possible. Time is heart muscle. The quicker you get attention, the better off your heart muscle will be (i.e., minimising damage to the myocardium).
Whilst I cannot give you specific recommendations for your exercise since I do not know every detail of your medical history or your recent hospitalisation, I would suggest speaking to your doctor and asking him the following questions:
1) Was there any damage to your heart muscle?
2) If there was damage to your heart muscle, what is your current ejection fraction? This will give an indicator of your heart’s pumping ability.
3) If you had a post-surgery treadmill test, what was your peak workload (speed and grade)?
The other thing is that you are nearly a year post-stent. This is a good thing because you have had time to heal and recover. Provided you do not have any issues with your blood pressure going too high (are you on beta-blocker medications?) or other medical issues which might affect your ability to exercise, then doing light cycling probably won’t hurt you and will, in fact, likely be good for you. But ultimately the final approval must come from your cardiologist who is familiar with your specific medical history and surgeries.
Hope this helps.
Warm regards,
Bill
Hi Doctor Bill,
Thank you for your quick response and sincere reply.
I will surely follow your guidance and seek my cardiologist advice by asking reply to your question before deciding for light bi-cycling.
Kind regards,
Sudhir Sharma
This is so thorough and excellent. Much appreciated on day 6 after stent placement and early mild heart attack. I could find nothing near this much help and it will be so very helpful. Thank you Dr. Bill. Thanks again.
Thanks for your comment Su. I really appreciate the feedback. If you think there’s anything missing or any ways I can improve on it, always feel free to write me or leave a comment. Best wishes for your recovery! Kind regards, Bill
Bill,
Great article, thanks much for writing it. Quick background — 52 years old, minor heart attack a month ago, 3 stents, post stress test last week my cardiologist said I was an excellent candidate for cardio rehab, have no apparent heart damage. My question is, do I really need to go through the hand holding of cardio rehab or can I just start going back to the gym? Hell, I know what I have to do — eat less, exercise more, and drink much less beer (yes, I know to start back slowly at first, but unlike your other readers I am by no means a fitness enthusiast, I just plug away because it has to be done). I really don’t need (or want) the remedial nutritional advice based on 20 year old guidelines, happy/sad faces to describe my emotional well being, etc. My biggest concern was another heart attack, but according to my doctor that is not very likely and if it does happen it will be massive and thorough. Somehow that is very liberating, not having to worry about trivial aches and pains. Anyway, so doesn’t it make more sense to invest my copay in a good personal trainer and get on with things? Or is there really value in going through a three month program?
Best regards,
Dave
Hi Dave, You sound like you’re doing great! Congrats! As for cardiac rehab, I’ll say this. If they use telemetry monitoring, then that will be VERY helpful for you to check your heart’s response to different types of exercise at different intensities. Sometimes the heart is on its best behaviour when the doc is there, but it can do funky things at other times when nobody is looking. So let’s say you do 6 sessions of cardiac rehab. That should be enough to know if your ticker is going to be cooperating with different types and intensities of exercise. If you’re going to hire a trainer, make sure they have experience working with people with heart conditions. I train personal trainers on how to work with people with heart problems and most of them at the beginning of the seminar look at me like “oh sh*t, what do I do with this guy who’s had a heart attack and surgery?!” I would strongly encourage you to do your diligence with finding the right person (or hire an exercise physiologist with experience with cardiac clients).
Bottom line: I think a cardiac rehab program for at least a month could give you a lot more confidence and knowledge about your heart and ways to keep it strong (plus finding any potential arrhythmias or other hidden stuff that might not have shown up during your stress test).
Hope this helps.
Cheers,
Bill
Cool, thanks very much, great advice. Appreciate it.
Dr. Bill,
Thank you for the helpful information. I’m 64, eat healthy, have never smoked and am somewhat of a workout nut with cardio and weightlifting and won a few bodybuilding contests at 63. Low body fat, 5’7″ and 168 pounds. Since I was adopted I know nothing about my birth parents other than my birth father died of a heart attack while waiting at a bus stop when he was in his 60’s. He smoked and was overweight.. Eleven days ago I had two stents put in the LAD and went into cardiac arrest during the procedure. I was told the LAD was 80% blocked but the other arteries were “normal.” I didn’t ask what “normal” was. Not sure how much damage there is to the heart yet, because I’m with Kaiser and my cardiologist there was not the doctor who put in the stents at another hospital and I was probably too out of it to ask all the right questions. My assigned cardiologist spoke with me briefly before discharge but I won’t be seeing her for two more weeks. I’m on a beta blocker, a statin and blood thinners. I’m anxious to get back to the gym. Do I start with the cardio and wait for the weights? How would I know if I’m doing too much? Any advice?
Hi Howard,
Thanks for taking the time to leave a comment and share your story. The biggest thing that sticks out to me is that you are only 11 days post-op since your cardiac arrest and surgery. You still have some healing to do on the inside, particularly if there was any damage to your heart muscle. Did they give you any troponin numbers? Any echocardiogram reports that state anything about wall motion abnormalities? Provided you have clearance from your cardiologist, you should be ok to do low level activities like walking until you go back for your check up (usually after a month). At that point, you might consider requesting a treadmill stress test to see how your heart looks on the ECG under high intensity exercise. If that comes back normal then your doc might give you the clearance to get back to weight lifting and higher intensity cardio.
As for your meds, whilst I confess I’m not a fan of pumping people full of drugs, in this case, the cocktail of meds they have you on are quite common after heart attack/angioplasty/stent. What blood thinner are you on? Clopidogrel (Plavix)? As for the beta-blocker, remember that it will lower your resting and exercise heart rate so even if you’re working at higher intensities (once given clearance to do so), then your heart rate probably won’t climb to it’s usual rate that it was when you weren’t on the meds.
As for knowing if you’re doing too much, make sure you’re paying attention to any signs or symptoms like I listed in my article (shortness of breath, tightness in the chest, pressure, etc). If you had symptoms during your last episode, there is a possibility future symptoms could be the same.
The bottom line at this point is to give yourself an opportunity to recover. Even if you feel well, there is still some healing happening on the inside. Once you get the final clearance from your doc, it might even be a good idea to do cardiac rehab for at least a month. They can put you on a telemetry monitoring system and see if anything is happening with your ticker whilst doing exercises consistent with what you’d be doing on your own at the gym. Remember, when it comes to the heart after angioplasty/stent, you have to train smart and be on the look out for signs and symptoms. If you do that, you’ll probably be ok.
Hope this helps.
Best wishes,
Bill
Thank you very much. I haven’t heard the word troponin before so I will ask. I had many echocardiograms but nobody told me of the results which I take to mean there was nothing abnormal. I am on Plavix, Lopressor, Lisonopril and Lipitor. Your site is quite helpful. My checkup is set for a month post op.
Hi Howard, it seems like they’re doing everything right. I would suggest googling “ejection fraction” too. If you had any myocardial damage, it may be reflected in the ejection fraction, but hopefully all good. Feel free to drop in and leave another message as you progress.
Cheers
Bill
Dr. Bill,
I saw my cardiologist and asked about the ejection fraction. What I recall her saying was that “normal” is 60 and I was between 40 and 50. Not really sure what that means. She also told me the heart repairs itself over time. She cleared me to start weight training again but not skiing right now. I had this fleeting thought of entering another national bodybuilding competition in July, but don’t know if with the loss of muscle weight I should bother trying! Whereas I had problem getting from 160 to 155 to make weight last July, today I’m 157.
Hi Howard,
Thanks for getting back to me. Good to see you followed up with your cardiologist. Regarding your ejection fraction, the norm ranges between 55 to 70% on average so if you’re between 40 and 50% then that means you had some mild damage to your heart muscle. You can read more on this here: https://my.clevelandclinic.org/health/articles/16950-ejection-fraction
Your heart will remodel to some extent but it’s different for every person. If you had what’s known as “stunned myocardium” then it can regain a fair bit of its contractile abilities. If you had a massive heart attack that blew out most of your heart muscle (which it doesn’t sound like applies to you), then it will be difficult to regain much function.
I can’t advise you on the bodybuilding decision, but hey, it would make a great comeback story!
Kind regards,
Bill
Dr. Bill,
New inquiry that may be a bit “off topic” but it’s relating to rehab after heart attacks.. Since my heart attack 6 weeks ago my libido has completely disappeared. Being aroused is not only difficult, it messes up my head. I was on testosterone replacement therapy under a doctor’s supervision for four years. It improved my mood, my sex life, my body fat and overall sense of well-being. I had my blood and levels monitored and donated blood twice a year so that the blood would stay thin and to avoid the risk of a stroke. I stopped the weekly injections right after my heart attack on January 24 and only recently started resistance training again. So now I wonder if the lower testosterone level and the meds I’m on have doomed me from one of the great pleasures of life at 64. Do you have an opinion about that or resuming the TRT. There are different opinions on the subject.
Hi Howard,
Thanks for your comment. You’re definitely not on an island all your own. I’ve heard of this sort of thing before. Remember that it’s still early days and your body is going through some adjustments. I would suggest speaking to both your doc that prescribed you the TRT and your cardiologist (and perhaps try to get them communicating so they can work together on getting your meds right). You might also find that over time you’ll be able to whittle down the dosages on your meds (as your doc’s discretion). Sorry I can’t be of more help, but I do think you raise an interesting point from which others might benefit. Please stop back and give us an update as things transpire. Best wishes, Bill
Dr. Sukala,
Thanks for your column. I had two stents in my heart in 2013(within 30 min.) after I had a heart attack. I was wondering if there is a maximum amount of cholesterol (bad) that a person’s heart can tolerate. My weight is close to my BMI range, and I exercise two to three times a week, plus practice Martial arts (no sparring), plus I eat a light breakfast, and lunch, and more at supper time. I am currently taking a b/p med, and an anti-cholesterol med. I love to jog in warmer weather, and hike when I get the chance.
Thanks, MH
Hi Mark, Thanks for taking the time to leave a comment. Cholesterol is one of those “it depends” sorts of things. There are some people with anomalously high amounts of cholesterol that do not have any vascular problems (be it the coronary or carotid arteries). Then there are people with low to normal cholesterol that still manage to have heart attacks or stroke. There is a genetic component and lots of factors and meta factors that can influence what constitutes a dangerous cholesterol level for an individual. There is a lot of debate on cholesterol and its role in the development of atherosclerosis. One thing we do know is that it’s at the scene of the crime, but we can’t necessarily say we 100% understand its role in the process. Best bet for you is to keep up with your healthy lifestyle. Cholesterol is only one piece of the puzzle. But we know that people who have a healthy lifestyle have lower blood pressure, better blood sugar levels, and a reduced overall risk of health problems. Keep up all the good work you’re doing and pay extra special attention for any signs or symptoms like those I highlighted in my article. I don’t want you to have any further problems, but if for any reason you do, you’ll be wise to get treatment asap. Hope this helps. Kind regards, Bill
Dr. Bill S.,
Thanks for the information. I had an MI in 2013, and in 30 min. had two stents put in. I take b/p med, and anti-cholesterol med. I was wondering if there is a maximum amount of bad cholesterol I am allowed? i eat a light breakfast, and a light lunch, and eat more in the evening. I exercise 2-3 times a week, and practice martial arts once a week (no sparring).
Thanks,
Mark
Hi Mark, Thanks for your comment. Sorry for the delay in responding. Your comment ended up in the spam folder for some reason. Nevertheless, I have rescued it and am responding below.
I think it’s important to note that the great cholesterol debate is not a clear-cut one. I’ve seen people with normal cholesterol have heart attacks and people with bad cholesterol get away with no heart attack. There appears to be a genetic component to cholesterol levels where they tend to gravitate in a certain range which can vary from person to person. With lifestyle changes (i.e., diet, activity, etc), cholesterol levels can improve but will likely still hover within that range (unless artificially manipulating it with meds as appears to be your case). The threshold at which blood lipids cause health problems will also vary from person to person. We also understand that inflammation plays a factor in atherosclerosis too, so this could be a contributing factor that partially explains the variance from person to person. Also consider your HDL cholesterol and the protective role it plays. I wish it was a cut and dry case, but unfortunately it’s not.
In answer to your question, I would suggest that you have a talk with your cardiologist regarding your LDL cholesterol profile and ask him/her what he/she thinks would be a suitable upper level for your individual situation. I cannot be more specific since 1) I’m an exercise physiologist and not a cardiologist; and 2) I’m not familiar with your entire medical history so could not legally give you any advice beyond general info that you can discuss with your doctor.
Kind regards,
Bill
Dear Dr. Bill
I am 59 now. I am a very happy and joyful person as told by my friends and family. I had a chest pain in right side of my chest during April 2006 and after angiography I was told that my two arteries i.e LCD & LCX are blocked upto 70 & 90% respectively. As per advice of my cardiologist I had got two stents on 10.05.2006. Since then I am regularly doing my morning walk upto 45-60 Minutes at least 6 days a week. Now for last 4 months I am doing some aerobic exercise for about 30 minutes before morning walk. I am getting regular check up with my doctor at Kolkata, India. I was a smoker before April,2006 but after that I left smoking completely. Now for last one year I do take two three cigarettes daily. Please suggest me to do still better in my life and lead a healthy life.
Thanking you.
Krishna Pratap,
Kolkata, INDIA
Hi Krishna, you sound like you’re on the right track. But if you can find a smoking cessation provider to help you stop smoking, that will help you significantly. Keep up with your exercise. That is a step in the right direction! Cheers, Bill
Thank you Dr. Bill for your kind reply of my query. I shall definitely try to reduce the habit and bring it to zero through my conviction. God bless you for your such a noble care of heart patient.
Krishna
Dear Krishna, thank you for your kind words. You’re on the right track. I believe working on strategies for quitting smoking will greatly protect you and reduce your risk of having any future heart problems. Remember life is a marathon and you just need to take small steps each day to win the race. Keep smiling ☺
Warm regards
Bill
Hi Dr Sukala great article wish more cardiologists would do this So my story is i’m 42 and I too had a HA in sept last year. Had 2 Des stents in my RCA. Cardiologist said i possibly caused it through cycling with a 70% plaque which ruptured due to the extreme intensities during cycling, dehydration etc. Had a Bruce protocol stress test 1 month later where i achieved 15.5 mins before i got nervous and stopped. Was on a 2.5mg of bisoporol then but now am off them as cardiologist says no real need as no damage and excellent LVF. Always played sports(football, martial arts, tennis, running, cycling, weight lifting) and always very competitive which they say helped me live due to the collaterals but i also question did it also do the damage in inflammation as i tried to train almost eveyday ? Now though i am nervous to perform any strenuous activity but was thinking about just doing weights? Lost over 10kg in a couple of months due to change of diet to Dr esselstyn’s. All of it is driving me and mrs nuts as so many conflicting things out there. On ramipril atm and about to start 10mg of simvastatin both low does just for protection. I’ve been discharged from rehab although they didn’t like my HR going as high as it did and not come back down but a lot of that was anxiety which I’m having counselling for and its really helped.
I still struggle about beginning the statin since my levels are good now and I’m still working on getting back to exercising. One thing though after my HA I started hearing my heart beat in my left ear and it’s worse after I take my plavix and aspirin and whenever I eat a meal. Any thoughts my doc says ignore it ?
So thats my story and really glad all the people above posted their stories they are very encouraging and wish them all the best.
Thanks for your comment Rav. I’m not sure about hearing your heart beat in your left ear. I know what you’re talking about but not certain it would have any relationship with your ongoing cardiovascular risk. I think from here on out, your best plan of attack is to work together with your cardiologist and keep up with your healthy lifestyle. Thanks again for sharing your story! Kind regards, Bill
Hi Dr Bill! I had a major heart attack 3yrs back. Got an angioplasty done with one stent in my left main artery. Currently the right main artery is still blocked 100%. My ef went down and is now 35%. I walk daily for 45 min. Do some body weight exercise for 5 to 10 min. I wish to practice martial arts. Is it advisable? I am now 32 years old.
Regards,
Mithil
Hi Mithil, thanks for your comment. If your right coronary artery is 100% blocked, I’d strongly recommended that you speak to your cardiologist about your exercise limits (in terms of intensity) and perhaps participate in a guided cardiac rehabilitation program. As you’ll notice from many of my responses, I cannot provide any specific recommendations to anyone since I’m not familiar with the fine details of each person’s health history. The big question in your case is if you’re symptomatic given your RCA is 100% blocked as you say. The other question is if you have collateral circulation around the blockage. Are there any plans for doing another angioplasty? The bottom line is that you need to be working closely with your doc regarding possible treatment options and safety limitations on your activity levels. Hope this helps give you some guidance.
Kind regards, Bill
Dr. Sukala
I had two heart attacks two years ago as a result I have two stents. I am 41 years old I have been weight training religiously three to five days a week for the last 22 years. After my heart attacks I lost 60% mass and 75% of my strength. I went through rehab and got cleared to workout but they do not want my heart rate going above 120. Which is 5.0 on the treadmill and they don’t want me lifting heavy. When I asked how heavy they really didn’t have a clue and told not to lift more than 65% of my max 10yrs ago EVER. Most of the questions I ask my cardiologist he can’t answer because he has admitted he does know how to answer them. I am his only patient under the age of 60 and non of his patients are a gym nut like me. I have looked and looked on the net to find answers for my training question, like how to weight train without over stressing my heart and will I ever be able to run and get my heart rate higher than 120bpm. I can’t find anything, everything is gear to the 65+ who are not gym nuts. I am not on beta blockers anymore and haven’t been for 4 months. Can you help me or point me in the right direction?
Thanks Matt
Hi Matt,
Thanks for your comment. I can certainly understand your frustration and, trust me, you’re not the first person to have this issue. Whilst I can’t necessarily give you any specific advice since I’m not familiar with every nuance of your particular medical history, there are some things you can discuss with your cardiologist in hopes you can get back to exercising at higher intensities.
1) You state you had two heart attacks. Was there any damage to you heart muscle? Did they run any tests on you to determine what your ejection fraction is? If you had a lot of damage to the heart muscle, then this can work against you. If you had no damage to your heart muscle, then you’re far better off than someone who had a full blow-out. A normal ejection fraction is around 50 to 75% but if you’ve had some damage and you’re down in the low 40s or less, then that could pose an issue with your ability to perform high intensity workloads (i.e., your heart is not as effective as a pump and it could plausibly lead to symptoms like shortness of breath).
2) Have you had a full treadmill stress test? In your particular case, you are used to living an active lifestyle and doing higher intensity exercise. I’d suggest speaking to your doc about arranging one of these to see 1) how hard can you exercise; 2) does your heart rate and blood pressure rise normally with graded exercise, and how high do they climb? If you’re on beta-blockers or any other meds that affect your HR and BP, then you might have a blunted response; 3) are you symptomatic in any way shape or form during high intensity exercise? and 4) how do you fare in recovery? Does your HR and BP gradually decrease back to resting levels in a reasonably short period of time (within a few minutes)?
3) You might also discuss with your doc whether or not there are certain meds that could make it safer for you to tolerate higher workloads. I’m admittedly not a fan of pumping people full of meds, but I do recognise that there are times where it’s medically warranted. For people with high HR and BP, exercise can send them both off into the stratosphere which can increase the risk of having another heart attack.
I think the bottom line for you is 1) can you do high intensity workloads without any abnormal responses (HR, BP, or any signs or symptoms); and 2) are there any specific reasons in your case, having a history of regular exercise, why doing high intensity exercise is medically contra-indicated?
I have worked with patients who had really bad congestive heart failure yet were still able to tolerate some pretty gruelling exercise due to peripheral adaptations. In other words, their hearts were badly damaged and had a low ejection fraction, but the rest of the body was very fit and efficient at extracting oxygen and nutrients from the blood (to compensate for the heart).
There is hope, but I think you just need to work with your medical management team to discuss your particular situation.
Hope this helps.
Kind regards,
Bill
Dr. Sukala,
After showing signs of a low risk abnormality on a stress test on 2/5/16, my cardiologist performed an angioplasty on 3/3/16 and placed 4 stents in my heart. I am 68 years old and have never had a heart attack or any angina pain. At first I was thankful for the stents but after reading several articles on the internet maybe they were not a good idea. (too late now) My doctor said that I was a prime candidate for the “widow maker” event.
Below is the summary from my cardiologist.
1. 90% proximal to mid left anterior descending stenosis successfully stented.
2. 90% proximal and 70% mid vessel stenoses in the right coronary artery successfully stented.
3. 90% distal right coronary artery successfully stented.
4. Normal left ventricular systolic function and wall motion with ejection fraction of 70%.
DISCUSSION: The intermediate ventricular branch may cause some difficulty in the future. I would recommend following it by serial myocardial perfusion imaging studies, since he has remarkably silent myocardial ischemia even with near global ischemia.
Can you reassure me that the stents were a good thing?
Thanks,
Bill
Hi Bill,
First thing I’ll say is you have to be very careful with generic info from the internet. I’m sure you can find articles that would scare the heck out of you or reassure you. I think to put it into perspective, every person’s clinical picture is different and must be treated individually. Based on the info you’ve provided, you certainly did have a lot of blockages in key arteries. The good news is that they were all found in time. For many people, the first sign of heart trouble is sudden death. So in your case, you didn’t have a heart problem. You had a plumbing problem. Your options would have been angioplasty with stents or open heart surgery. The first option is the least invasive and has a quicker recovery, not to mention less trauma on the body. The fact that you still have an ejection fraction of 70% is excellent. Without knowing all the nitty gritty details of your medical history, I think what the doc did for you seems consistent with what I’ve seen for other patients in similar situations. Honestly, you’re a very fortunate man that they found all this when they did. It was only a matter of time til the volcano erupted. Hope this helps. Kind regards, Bill
Thank you very much for your response. I have learned how fortunate I am and will enjoy each and every day of my extended life.
Thanks again and great site!
Bill
i am 65 yrs male,i under went angioplasty 2 years back and doctors fitted 4 stents…i do walking evryday,i also do yogaasanas for 30 mins…i am 183 cms tall and weight is 83 kgs…can i take viagra once in week.thanks
Hi Subhaschandra, Viagra can cause a reduction in blood pressure by making your blood vessels dilate. If you’re taking other medications that lower blood pressure, then you’ll need to be careful. I’d suggest speaking to your cardiologist about this as he/she will be familiar with your entire medical history and can properly advise you on this.
Dear Dr. Sukala
I am a 53 year old male. I had 3 stents placed in January of 2015. Two in the LAD and one in the OM. Lad was 90% blocked. I have a third small artery that is less then 50% blocked. I exercised for many years prior mostly weight training pretty heavy right up until I had an episode, bench press 280 plus ect. I went through 6 months of Cardio rehab heavy cardio only training and I am still on a maintenance at the hospital rehab 2 to three days a week. Have a great new diet and life style lost 30 lbs. and all meds bata blocker, Benicar, cut in half still on Effient, and Aspirin. I developed a good case of anxiety for 6 months made me have multiple false alarm cardiac symptoms that sent me to ER. Was given multiple types of stress tests and finally a second cath. to check stents after 9 months. Given clean bill of heart health for my exercise and I see a Therapist for the anxiety which is under control. Never had a heart attack no muscle damage.
I have started to weight train again my questions is what effect does this have on my heart has I train. How does it differ from my heavy cardio in terms of effect on blood pressure and on the stents. I am cleared for 140 to 145 heart rate. I use moderate dumbbells as compared to prior to stents. Occasionally I feel a little light headed but not dizzy towards the end my strength workout at the last set ect. It does not happen all the time. I have no chest pain or shortness of breath and heart rate does not peak above 110 during lifting mostly stays in low 100’s or below. Heart rate recovery is excellent.
Thank you
Jerry
Hi Jerry,
Thanks for your comment and for providing a lot of detail about your medical history. As I say in nearly all of my responses, I cannot give you any sort of absolute “do this or do that” sort of advice, but I can give you some things to consider which you may wish to discuss with your cardiologist.
First and foremost, you pointed out that you did NOT have a heart attack so this is a good thing. Basically it means you had a plumbing problem and not a heart problem. If you had a heart attack with damage to the heart muscle itself, then you’d be in a different league altogether (depending on the level of damage).
Second, you mention that you had your angioplasty/stents done back in January of 2015, so you’re well over a year post-op now. It also sounds like you’ve been pretty active with your cardiac rehab program. THAT is the single most important thing you could do. In fact, I recommend cardiac rehab to fit people with heart problems because they WANT to get back to their routines asap. Having the close guidance of the cardiac rehab team gives you lots of specific information on your individual response to exercise. Having a good idea about your habitual heart rate and blood pressure response to exercise can be very valuable.
Third, you mention that you have a long history with resistance exercise so it’s not like you’ve been flat on your butt doing nothing for 40 years and then decided to go all out and get on a health kick. The fact that you have a good cardio base and experience with weight training puts you at an advantage over those who are completely inactive and have no experience with exercise. You are probably more in tune with your body and this can be valuable for gauging intensity and knowing when to cool your jets (from a safety standpoint).
Fourth, both cardio and weight training will increase your heart rate and blood pressure. Though you mention you’re on a beta-blocker. This will help keep your heart rate and blood pressure down a bit, depending on the dosage of course. I think if your cardiologist has run you through multiple stress tests and you are a year post-op, AND you have his full consent to return to reasonably strenuous exercise, then that is a good sign. Without saying “yes, go do this or that” I think that the weights you’re talking about (moderate dumbbells) and the heart rate limits you have set are all pragmatic and reasonable and do not appear to be too “out there.” If you’re still going to the cardiac rehab and they have weight training equipment there, perhaps you might like the team to check your blood pressure immediately after a set of, say, bench press. Heart rate is one piece of the puzzle, but it would be good for you to know what your individual blood pressure response is to a given resistance in both the supine and upright positions (i.e., a bench press on your back vs a chest press in the upright position on a machine). I would suggest trying to avoid any max lifts or extreme lifting where you’re only squeezing out a few reps. Those sorts of maximal efforts can potentially spike your blood pressure.
Bottom line: I’d say to speak with your cardiac rehab team and get specific advice from them regarding exactly how much you can or should lift and your individual blood pressure/heart rate response to given resistances.
Hope this helps. Thanks again for your comment.
Kind regards,
Bill
Hello Dr. Sukala,
Your articles are very helpful.
My name is Manjiri. My age is 39 years. I had a massive heart attack on 8 September, 2015 (early morning). It was 6 months back. I had a severe chest pain and then I fainted. My husband did pumping and I came to my senses. Still severe chest pain and breathlessness was there. I was immediately admitted and angiography detected only one block of 99%. Angiplasty was done immediately and I was saved by God’s grace.
Before this, I did not have any problem of high cholesterol, high BP. I was very active. I was taking walk and doing Yoga everyday. My 2 deliveries were normal. My weight was 55 kg. Doctor was also surprised that a person with such a good life-style can have this problem. My cardiologist said that it might be a genetic problem.
1.5 months after the angioplasty, my stress test was done and cardiologist said that I am fine and can go ahead with a regular walk (not running and jogging). Damage to heart is 10%. But my weight is reduced to 51 kg.
My questions are:-
1. What is a genetic problem?
2. 6 months before the heart attack, I had taken Ayurvedic treatment for migraine in which they made me drink half glass of ghee for 3 days. Could it be because of that?
3. My father is taking mild blood thinner since he had a chest pain some years ago.
4. My brother is also having a problem of deficiency of protein C and taking a mild blood thinner .
5. Is there any connection with this?
6. My pro-thombosis test is done and it is negative.
7. My weight of 51 kg is okay or I have to gain some more?
8. Which are signs that I should worry about?
9. Sometimes there is a tingling sensation in my both legs. I have a problem of vericose veins.
I still have some anxiety. While taking a walk, I am still not confident that I can walk more than 15 min. But I am doing my regular kitchen work and I am able to do it for an hour continuously without a break.
Back of the mind, there is always a fear that anything can happen to me at anytime. My cardiologist says that these are psychosomatic symptoms and I should just ignore them.
3 days before the heart attack, there was sudden pain in chest and left arm. But I thought that it might be because of indigestion. Which are symptoms I need to worry about? Should I go for another stress test?
Please advise.
Thanks in advance.
Hi Manjiri,
I’m sorry to hear you’re having anxiety after your heart attack. But rest assured, you are not alone. This is a very common reaction and in time you will probably start to feel comfortable again, but it takes time. In answer to your questions below:
1. What is a genetic problem?
Your cardiologist just means that your heart problems might be related to genetic factors. You are clearly doing your best to live a healthy lifestyle, and this is a good thing, but our genes cannot be directly controlled. The good news is that no matter what your genes are, you can significantly help yourself by keeping up your healthy lifestyle.
2. 6 months before the heart attack, I had taken Ayurvedic treatment for migraine in which they made me drink half glass of ghee for 3 days. Could it be because of that?
I can’t say exactly what caused your heart attack, but it’s improbable that something you did one time 6 months ago contributed directly to your heart problem.
3. My father is taking mild blood thinner since he had a chest pain some years ago.
4. My brother is also having a problem of deficiency of protein C and taking a mild blood thinner .
5. Is there any connection with this?
It is highly probably that you have a family history of heart problems if your father and brother are taking heart meds.
6. My pro-thombosis test is done and it is negative.
7. My weight of 51 kg is okay or I have to gain some more?
I can’t tell you what your ideal body weight should be since body composition is more important. If you can get a DEXA scan, then that will tell you how much fat you have and where it is located. That is more valuable than just a body weight on the scale.
8. Which are signs that I should worry about?
The main signs and symptoms you need to be aware of include chest pain, chest tightness, shortness of breath, pain in your back, jaw pain. These are your standard angina symptoms related to your heart. Everyone is a little different, but it might be worth speaking to your cardiologist for more specific information on your unique condition.
As for getting another stress test, you’ll need to speak to your doctor about this to see if it’s appropriate for your individual condition. If you’ve had one already and it came back looking normal (after your surgery) then this is a good sign. Your doctor would also have more information regarding your other arteries if he did an angioplasty on you.
9. Sometimes there is a tingling sensation in my both legs. I have a problem of varicose veins.
It’s hard to say what this is. I would suggest speaking to your doctor about this to get a proper diagnosis.
I’m sorry I can’t be of further help, but I cannot provide any specific advice or recommendations over the internet (ethically or legally).
Kind regards,
Bill
Thank you so much doctor for your valuable advice. I will do my best to get back on track.
Regards,
Manjiri
Hi Doc,
your article was informative and helped me to become relaxed …….unfortunate I did not get a lot of discussion before release….but I was told to do some life stile changes and to resume exercise……But not a lot of time was spent making me feel comfortable (that I did not have to be scared to move are lift my infant grand kids) after returning home…However after reading your article I feel empowered in my recovery and much more confident… I did not have a heart attack but my CIRC. artery was blocked and a metal stint was placed.
Thanks for giving me clearer insight and ammunition to assure I ask the right questions and observe the right warnings,
Thanks, Andrew M.
Hi Andrew,
Sorry for not responding til now. I’m only just seeing your comment. Thanks so much for the kind words and feedback. I really appreciate it. Just stay aware of any signs and symptoms and be sure to seek a consultation and treatment if something doesn’t feel quite right. People who pay attention to the signs and symptoms generally tend to have better prognosis than those who live in denial (that river in Africa!).
Kind regards,
Bill
Can you state how dangerous is the flu after an angioplasty?
Hi Abdullah,
Thank you for taking the time to leave a question. I think it’s important to note that the flu is dangerous to everyone at any age. I recently lost a dear friend to the flu who was only 35 years old and in excellent health. However, it’s important to note that, when looking at the statistics, the flu generally tends to be more dangerous to children and older adults who may be comparatively more physically weaker than healthy younger adults. If you have any underlying medical conditions that have weakened your immune system, then the flu could pose a greater risk.
In regards to your question, I have not heard a lot about a connection between the flu and angioplasty. For the most part, it may still be a case of having to consider the individual and his/her health status. But I did do a bit of digging and did come across something that might be of interest to you. Here is an article that discusses the importance of flu vaccinations in people who have recently had angioplasty.
And here is another general article on the flu and heart disease which might also provide some insight.
The bottom line: you should discuss this with your doctor to see if a flu shot is something that might be appropriate in your case.
Kind regards,
Bill
Re: Cost of Stent and Angioplasty
Dear Doctor
My name is Muhammad and I am age 59 years with the following illness:
1 Diabetes – 12 years
2 Paralyzed – 8 years
3 Kidney checkup quarterly – 4 Years
4 Angiography – Recently diagnosed ( But not yet )
5 Angioplasty – Next step
6 Heart bypass – Last step
So my medical history is above. Please advise me of the approximate cost of treatment and admission time. Thank you.
Hi Muhammad,
Thank you for your message. The cost of angioplasty with a stent is going to vary significantly from country to country and medical system to medical system. You’ll also have to consider that your individual health status could also play a role in how long you’ll be in the hospital and what the final cost might be. For example, if there are any complications due to other underlying health conditions, then this might keep you in the hospital for an extra day in order for the doctors to stabilise you and ensure you are safe to be discharged.
In general, and angioplasty might keep you in the hospital for 1 – 2 days. Every doctor is different and some will try to get you discharged as soon as possible where others might keep you in for observation for 2 days (or longer if any unforeseen complications).
The bottom line on cost is that you’ll need to discuss this with your local doctor and other relevant hospital administrators. Sorry I can’t provide a dollar figure for you.
Kind regards,
Bill
Dear Doctor,
How soon can I travel after angioplasty?
10hours air trip.
Hi James,
Thanks for your comment. The question of “how soon can I fly after angioplasty” is quite common. Ultimately you’d have to ask your cardiologist for a specific time frame since he/she’d be familiar with your particular situation. The wait will also depend on other health conditions related to the angioplasty/stent such as if you had a heart attack, have high or low BP, the medications you’re taking, etc. There is no cut and dry cookie cutter answer to this since there are so many mitigating factors around heart health and air travel. There are pressure changes in the cabin that could ultimately cause changes in HR and BP which might affect your body, but in my experience, cardiologists I’ve worked with have (generally) made sure patients waited at least a week, sometimes two weeks, depending on their particular health conditions. But again, I do need to reiterate, I cannot give anyone specific advice here on this topic since it genuinely does depend on the individual and their health issues. Hope this helps. Cheers, Bill
Hi Dr Bill, I’ve found your forum very informative, many thanks for putting people’s minds at rest.
My story is that I’m 48 years old and had a stent fitted in early January 2016. It followed a heart attack that felt more like a fever than any actual pain in the chest. The blockage was in a back artery but a scan done the next day showed no muscle damage done.
I have recovered well, I haven’t had a cigarette since it happened but have vaped when feeling stressed.
I know this is wrong and will try to stop inhaling completely. My stress hales from not being able to lose any weight. I feel enormous and believe I have low testosterone and high estrogen. I would like to know what I can do about this? I’ve started cycling and am finishing my cardio rehab shortly. I am going back to work next week and hope the extended working will burn more calories.
I really want to know if I can increase my testosterone by visiting the gym more. I know that if I could shed the weight my stress would diminish and my confidence (which since the heart attack had been seriously affected) would definitely increase.
Would really appreciate your view.
Many thanks
David A
Hi David,
Thanks for taking the time to leave a comment. A few things caught my attention here:
1) You state that there was no damage to your heart muscle. This is a very good sign. If you had damage to your heart muscle, then your recovery time and process would be a bit different.
2) You’re participating in cardiac rehab. This is another excellent sign. I would encourage you to take advantage of the staff and ask them as many questions as you can, given they are more familiar with your complete medical history than I am.
3) Cigarette smoking. I would encourage you to speak with your cardiac rehab team to see if they can refer you to a certified smoking cessation provider. Avoid all the quick-fix gimmicks out there that will likely not work in the long-term. If you continue to smoke, then it can increase your likelihood of having another heart attack.
4) Testosterone and estrogen levels. I would suggest getting a referral to an endocrinologist for further workup to measure your testosterone and estrogen levels. It might intuitively seem the case that your levels are low, and you could be right, but I would suggest having them properly measured to ensure that, in fact, the levels are off. Exercise can increase your testosterone levels, but I don’t think by itself it will be a large change. Nevertheless, it IS still a step in the right direction and will have a number of benefits that will improve your overall health and well-being (and give you more energy by default, independent of testosterone levels). I would suggest speaking to an endocrinologist about this and get as much reliable information as possible.
The other thing I noticed is that you mentioned your stress would diminish and your confidence would improve IF you lost the weight. I believe this is a piece of the puzzle, but it also opens you up to the tyranny of “I’ll be happy when…..” And then when you lose weight, you might find that things are not a whole heck a lot different. A lot of our happiness stems from our beliefs, some of which are true, and some of which deceive us. Does your cardiac rehab team have an on-site counsellor or social worker? It’s a good idea to sound off to someone with proper training in this area to help keep you on the right track.
Thanks again for taking the time to leave a comment, and i hope some of this was helpful in getting you back on track!
Kind regards,
Bill
Dr. Bill,
I’ve corresponded before but have new questions. Had the heart attack on 1/24. The LAD was 80% occluded and the others were clear. I had two stents. I’m on metoprolol, clopidogrel, lisinopril and baby aspirin. I’ve been doing resistance training cardio daily, initially for 30 minutes and now two sessions of 45 minutes daily as I’m preparing for a bodybuilding competition. I’m 5’7″ and 157 and age 64. I had an echocardiogram yesterday, am between 60 and 65 now and my cardiologist says I’m healed. I was on TRT for four years and stopped abruptly after the heart attack. Had my T tested and it’s now low at 185. I want to go back on it. My cardiologist won’t say yes or no but my out of network “anti-aging” doctor is currently out of town. I have done a lot of reading and the studies show no link between TRT and heart attacks. Strokes are something else, but I’m on a blood thinner. What is your opinion about resuming TRT?
Hi Howard,
Thanks for coming back and leaving another comment. Based on what you’ve provided, I take it your echo showed you had an ejection fraction between 60 and 65%. That is pretty darn good! Regarding your testosterone levels and the question of whether or not to go on replacement therapy, I will confess I haven’t done a lot of digging on this particular topic, but I did come across something that is relatively recent and might be worth discussing with your doctor: https://www.sciencedaily.com/releases/2015/11/151109160558.htm This study was based on 1472 men who were apparently healthy and found that TRT did not increase their cardiac risk. In all fairness, this is a single study, but I think it would be worth your while discussing this in depth with your anti-aging doc and cardiologist. It would be good to have some sort of convergence of opinion and something with which you feel comfortable. Sorry I can’t be of further assistance, but am hopeful this is helpful to some extent. Kind regards, Bill
Hi Dr Sukala
Great article and outstanding effort in answering all the questions out there. I am male , 42 and from the UK. I had a heart attack on 7 Sept 2015 had 2 stents in my RCA, with no apparent damage shown in echo. I had a stress test 1 month later bruce protocol in which I achieved 15.5 mins and given the all clear to participate in what i wanted.
I have always been very active, diet was bad in my younger years although last 5 years it has been fairly clean so came as a big shock when this happened. I had symptoms that something was wrong only through Jaw pains but neglected to correlate them to a heart problem since they only occurred when i was doing high intensity exercises. The pain was so mild and would subside instantly as i slowed down. However one day the plaque broke and occluded the artery. There was alot of emphasis on my cholesterol which was TC 5.2, Ldl 3.5 and Hdl 1.3 at the time which i think is average but i’ve read so much about statins and diet that I am convinced no one really knows what to say at this present time. Is it sugar, Saturated fats, too much exercise, Stress, genetics, Omega 6 vs 3 the list goes on with so many knowledgeable people and so many differences in opinion. I took myself off the statins as I became Vegan which kept the numbers very low and i’m experimenting with what i can add to keep them within the levels suggested by my Drs of Ldl < 2.4. I loved my sports but since the stents ive been scared to go back to what i did before, just in fear of damaging the stent. What kind of sports would you advise against ? I like football, Tennis, cycling, running and weight lifting. Should I fear high heart rates given the all clear? My medication today are baby aspirin, clopedigrel, Ramipril 1.25. Appreciate any advice or info you can give. All the best to everyone its a tough time but dont be afraid to ask questions and get help from a counsellor if you need to. I did and it made a huge difference to my life.
Hi Rav,
Thanks for taking the time to leave a comment sharing your story. It looks like some of those bad habits from your earlier years caught up to you, but this doesn’t mean it’s the end of the game. Far from it. You do have a lot more that you can control (i.e., lifestyle) than what you can’t control (i.e., genetics).
I’ll point out a few things here for you and other readers which I think might be helpful. I certainly understand your point regarding all the confusion about cholesterol, statins, and all the other factors that contribute to health. When I hear people ask, “why can’t you experts all agree on one thing?” Actually, the truth is that most legitimate experts DO agree on the same thing, but we now have a massive proliferation of pseudo health “professionals” spouting off all kinds of rubbish on social media yet they have no health qualifications and are unable to read clinical research reports to inform their opinions.
To settle this, cholesterol is indeed a fickle one, but probably not as fickle as everyone might think. I have seen people eating extremely clean yet still had high cholesterol due to genetic influences (i.e., familial hypercholesterolemia). I have also seen people who eat complete rubbish diets that still managed to have low total and LDL cholesterol and high HDL cholesterol, the latter of which is protective. On that note, cholesterol levels tend to fall within a certain range for people and can be mildly influenced for better or worse through all the lifestyle factors (i.e., diet, exercise, smoking, background physical activity, etc).
Looking at the list you’ve provided (sugar, saturated fat, too much exercise, stress, genetics, omega 6 vs omega 3 etc), it is fair to say that the devil is in the dose for most things. If you overdose on all these things on a regular basis, it will obviously pollute your health in many ways not just related to cardiac health, but can impact your risk of cancer among other things.
You mention that you took up a vegan diet. If that works for you and it is sustainable for the long-term, then that’s a good thing that’s right for you. Not everyone wants to go that route, and that’s ok for them, but the biggest thing is each person finding strategies that work for them. I also recommend a Mediterranean style diet for people after they’ve had heart troubles, as it is a nutrient-rich diet that is recommends good quality veggie intake and monounsaturated fats.
As for what you can and can’t do, ultimately the best person to discuss this with would be your doc. If you are around 8 to 9 months post stent, then I can’t imagine you would damage the stent at this point. I’ve never heard of it being an issue in any of the patients I’ve worked with in cardiac rehab. However, I think if you were still pretty fresh out of your surgery and were back at the gym pumping iron and doing high intensity exercise, then the rise in blood pressure could create some instability and possibly cause trouble for that stent (as it wouldn’t be fully set yet).
If you’ve had a stress test and tolerated 15.5 minutes, then that is a good sign that you should be able to get back to doing most sports. Plus that, you are taking aspirin, a blood platelet inhibitor, and an ACE inhibitor. The combination of all this information should be viewed as reassuring, plus if your cardiologist has cleared you for exercise then you should be ok. I would recommend just being vigilant about any signs and symptoms in the future. So if you have any other indicators of jaw pain, chest pain, etc, then you need to get to your doctor as soon as possible for further work up.
In closing, you’re going to have a pretty hard time killing yourself if you’ve ticked all the safety boxes (clear stress test, patent stents, vegan diet, meds, and watching for any signs/symptoms). Try to live your life and live it well and not worry too much about things unless you have a real reason to be concerned (i.e., chest pain, jaw pain, etc). If you’re not sure, then go to the doc and have it checked to rule out that it’s of cardiac origin. If you do all that, then I’m sure you’ll be fine!
Hope this helps!
Kind regards,
Bill
Thankyou so much for taking the time to answer my queries
Dear Dr Bill, I am an army officer and have my regular exercises. I was admitted in the hospital on 15th of Jun this year with severe chest pain. Two days later i had an angiogram which showed 99% block at LAD and another 45% block at RCX. Dr also noticed the 3rd block at RCA which is about 25%. They did place a DLE stent on the LAD and left other two unattended. Today I returned home. I did have high cholestorol and hypertension for the last 8 to 10 years and was under medication (aspirin 75mg, Osartil 50 mg and Rosuvastatin 5mg). My blood sugar level is normal. I have family history related to cardiac problems.
My cardiologist did not give me any advice on physical activities or rehab program except advising me for taking regular medicine from now on. I am 48. I am worried about the two other blocks those were left unattended by the cardiologist. I am also confused about my lifestyle for future days to come. When and how should I start my exercises, duration and frequency etc. Eagerly waiting for valuable guidelines. Best regards.
Hi Colonel Sharif,
Thank you for writing. As I’m sure you can appreciate, I cannot give specific guidelines since I am not completely aware of your entire medical history. But the general guidelines that I’ve provided in my article are a good start to get you going.
Regarding your other arteries that are 25% blocked, they generally do not tend to cause any problems until about 75% or higher. Some docs feel that intervening in low grade blockages could pose an unnecessary surgical risk for something that isn’t going to cause you problems right here and now.
I would suggest you speak with your doctor and have a treadmill stress test done to see what your exercise capacity is. From that, you can work with your doctor to determine a safe level of exercise that you can do on your own. It will also give you both some reassurance that your heart is stable and there are no other issues which could cause problems (such as arrhythmias).
Regarding timing of your exercise, remember that you are still fresh out of surgery so there is still healing happening on the inside even if you feel well. Once you receive final clearance from your cardiologist (perhaps 2-3 weeks, maybe 4), then you can get back to starting off with low level walking on flat ground to rebuild your fitness.
To recap, I’d suggest the following:
1) Get a treadmill stress test done by your cardiologist
2) Ensure your heart is stable and there are no other issues which could be worsened by exercise
3) Get final clearance from your doctor
4) Start off with low level walking as I’ve outlined in my article
5) Then progress to the higher levels (as I’ve outlined).
Again, please be advised, I do not provide specific medical advice or guidelines on my website. If you can find an exercise physiologist in your area, then that could be a good avenue to get specific guidelines. Hope this helps give you some direction.
Kind regards,
Bill
Hi Bill,
I had one stent placed four days ago. The blockage was 80%. Another artery at 40% was not stented. No heart attack, just mild discomfort that prompted me to seek help. At 81, I am not into heavy workouts but I do try to do a 1/2 hour on my treadmill every day (3 mph @ 10%) at keep active plus some light weights. Good diet, non smoker etc, but I do feel quite weak. BMI is 27. I am not sure if the weakness could be drug related (ramipril, diltiazem, Plavix, aspirin and Crestor) or a normal result following the procedure. Your thoughts would be appreciated.
Thank you kindly,
Barry McIntosh
PS I did have Afib five years ago but that was cured with ablation and never have returned
Hi Barry,
The good news is that you did not have a heart attack. This means you had a plumbing problem that was caught in time. Regarding feeling weak, I would suggest discussing this with your doctor, as he/she is most familiar with your unique situation. If the medications you are taking are new to you, then it is plausible that they could be making you feel a bit low on energy. The Ramipril is an ACE inhibitor which can lower blood pressure and possibly sap your energy a little bit. But also remember that you are only 4 days post op, and it’s quite normal to feel tired after all that excitement. But again, the bottom line is to maintain good communication with your doctor and work together to find the best approach that makes you feel your best. Hope this helps. Best wishes, Bill
Dr. Bill,
I stumbled on this trolling for opinions on whether to do a cardio rehab program. After a series of tests, including passing a 12 min stress test, ecko, and nuclear test, my CT Angiogram showed multi vessel CAD.
No heart attack, damage, just fatigue and some angina pains. Bouts with fluctuating BP, and occasional SOB.
Got two medicated stents in RCA. Center and Right have 70 % blockages, but doc “measured them and it showed good blood flow. Big family history. I’m still in denial. I’m 62 and the only one who didn’t have “something” wrong.
In my mind I’m leery of the other 2 blockages and wondering if they could be stented on my “insistence” for peace of mind. They say the LCA provides 2/3 of the goodies.
I’m also going to take a money hit by doing the program. I thought maybe to do half and drop out just for the education. I went back to work on Day 3 post op and have been walking 20 to 30 min a day ever since.
Should more stents for the other 2 places being a consideration, or am I just being impatient. Stents on Jun 14th this year.
It has always seemed for many years even my ice hockey days I would always be SOB until I warmed up. Is this because of CAD?
thx
Hi Brian, the decision to stent or not will ultimately be up to your doc and will be based upon the extent of the blockage(s). In my experience, many cardiologists start considering stenting as an option at about the 70% blockage stage. That’s the point where people start experiencing symptoms. The other consideration is whether or not to take a risk with surgery if it can be medically managed without surgery (i.e., there’s nothing routine about routine surgery). As for cardiac rehab, having worked in cardiac rehab, I think you’ll find it helpful, but whether you complete the whole thing is up to you. Not sure if you’re US based, but I know the healthcare system there is irreparably broken re: health insurance coverage and out of pocket expenses. When I worked at a hospital in San Diego, I used to wrestle with insurance companies in a daily basis to get my patients covered. I’m sure it’s no better now. But anyway, if it’s in the budget, I would recommend a cardiac rehab program for sure. As for your SOB, if you had this near the time of your stents, then it is plausible it could have been to do with CAD, but can’t be certain. Hope this helps.
Thanks for your reply. I’m in Massachusetts, USA. I think because I have CAD, I wonder about the efficacy of “busting butt”, but perhaps I should at least try some sessions and then I will know where my threshold is.
I am of course concerned about the other blockages, and will discuss at my 3 month follow up. I think the US Healthcare system and the “rules” of the insurance companies and payouts drive how much / or how little a doc might do. I know he had a tough time doing just these 2 and you can only stay in there so long with the dye as it will shut down your kidneys!
I’m mad at myself for not pushing this full work up earlier in my life. Could have been there for YEARS. BUT I also as I stated discovered the walking stress test , even with nuclear proves nothing.
Had I not had the CT angiogram , or the cath, I would have been just “trying harder” to get in shape…………….was even considering going back to ice hockey in a “fun” league or pick up this winter. So much for that.
Thanks again for an unbiased opinion. I will be exploring my options in the coming months.
BTW, am I the only one with difficulties trying to submit posts with the CATCHA codes, keeps coming up with error when there is none
Brian
Hi Brian,
Yes, you are right about that. Fat balding insurance company bureaucrats with finance degrees are sitting in offices calling the shots about what docs can and cannot do. It’s been a problem for quite some time now. Nevertheless, glad that you were able to get to the bottom of things. If you didn’t have a heart attack then you had what could best be described as a plumbing problem. So you are in the better side of the exchange. Also, the fact that you had symptoms can be a good thing. At least you had warning signs. Not everyone gets clear enough symptoms that they can tell for themselves it’s a heart problem. Or if they do, they sometimes ignore the signs (denial) and end up with half their heart muscle blown out. That’s when the real problems kick in with reduced exercise capacity and, if a large heart attack, mild or moderate congestive heart failure.
Keep up with your proactive approach and you should be fine in the long run.
BTW, I’ll look into the captcha code. Have not had any other complaints.
Best wishes, Bill
Hi Bill,
I must say thankyou for replying to my previous inquiry. I don’t know how you find the time to reply to everyone. I had 2 stents fitted in January and have made a good recovery. The only thing that really needs some work is my diet. I’m just getting back into working and all the rehab exercise is over. I would like to try a Nutribullet diet but the small print says to consult with your doctor if you are on colesteral reducing drugs and blood thinning medication.
When I can afford a consultation with you, I will have one, but rather than list all my medications could you tell me why having healthy vegetable and fruit smoothies could mess with my medications.
Understand your busy but I would appreciate your thoughts.
Kind regards,
David Aylott
Hi David,
Thanks for your kind words. It sometimes takes a few days to get around to it, but I do make a good effort to be attentive to people who take the time to comment on my website. Most of these articles are now ranking highly in Google so I take personal pride in being able to help people with good information and fend off a lot of the social media Insta-Muppet “experts” that are confusing everyone with nonsense!
Regarding your question, in the grand scheme of things, I don’t believe that veggies and fruits should interact with your meds, but these types of juicer products generally have to put a broad disclaimer on it for the litigious subset of the population that wants to sue for stubbing their toe getting out of bed in the morning.
The thing to remember about juicers in general is that they tend to remove the fibre which can increase the sugar load of the juice. I recommend people eat the whole fruit or vegetable so that the digestive properties are “as nature intended.” Having said that, if you’re drinking a juice with a meal, that will moderate the rise in blood sugar a bit (as opposed to guzzling straight refined juice). If you have any issues with your blood sugars or are at risk of type 2 diabetes, then I’d recommend eating the whole food instead of its juiced version.
Hope this helps.
Bill
Hi Dr Bill Sukala This is Deepak and I am almost 60 years old. I had my 1st stent in 2009 and the 2nd one in 2016. I have been drinking alcohol for 40 years. I’m still drinking moderately. Is it going to make my heart worse? Please advise.
Hi Deepak,
As I tell everyone in the comments, I cannot give any medical advice here. First, I would suggest you discuss this with your doctor who is most familiar with your particular health history and any medications you might be prescribed. Alcohol does have effects on your health and it can interact with medications. But as with all things, the devil is in the dose. Obviously if you’re drinking a lot then, yes, there could be possible adverse effects on your heart. If you have other health conditions such as diabetes or high blood lipids, then alcohol is not going to do you any favours. Again, bottom line is that you should have a talk with your cardiologist or general practitioner about your particular health history and if drinking alcohol is going to affect your heart. Kind regards, Bill
Hi Sir, I’ve an angioplasty stene surgery on march 17 this year and I’ve 90/60 bp . This is my 2nd heart attack. I just want to know that when I’m going to do exercise and in future there will be any further heart attack for me or not .
Hi Srinibash,
I’m sorry to hear you’ve had a rough time with your heart. No one can guarantee you won’t have another heart attack, but you can certainly take steps to minimise the chances of having any more heart troubles. I cannot give you any specific medical advice, but I can suggest some things you can discuss with your doctor.
1) I would suggest discussing with you doctor the possibility of having a treadmill stress test done. This will help determine what your unique response to exercise is. With this information, you’ll then be able to figure out a safe workload you can perform when out on your own. Also ask what your blood pressure response is during exercise, as it is somewhat low at rest.
2) As your doctor if there was any heart damage or wall motion abnormalities. You need to see how your heart is functioning, as this can also help you determine how hard you should be exercising.
3) Discuss your medications with your doctor and the effects they will have on your ability to exercise. For example, medications like beta-blockers might make you feel a bit more tired and lethargic and that could make exercise feel more difficult.
4) Discuss your eating habits with a dietitian and get on a path to healthy eating (if you’re not already doing this).
Hope this helps you.
Kind regards,
Bill
Hi Dr Bill I’m a 51 year old female who had a massive heart attack this past January. I had a stent put in my RCA which I was told was 100percent blocked! I also have COPD. Im trying to change my eating habits and I want to start getting more exercise as well,but I’m tired so much of the time and I also get very winded very quickly! I live on the third floor so when I go out and come back in I’m so out of breath coming up the stairs even taking my time. I’m just not sure what to do or how to change all this! I’m also overweight I’m 5-4 and weigh about 185 lbs but I haven’t gotten under 175 lbs in years no matter what I do or dont do! Do you have any suggestions on how I can feel better and help my heart and my lungs at the same time?! I’d appreciate any advice you might have!
Thanks,
Your New Fan,Bobbi Jean
Hi Bobbi Jean,
While I cannot give any specific medical advice, here are some options that might point you in the right direction:
1) Speak to your doctor about your echocardiogram report and ask if there was any heart muscle damage. If so, how much? What is your ejection fraction? If you had a bit of damage, then I would recommend asking for a referral to a hospital-based cardiac rehab program to help you exercise safely and effectively under the watchful eyes of a trained team. This will help you set safe exercise guidelines specific to you.
2) Regarding reducing body fat (and losing weight), the best answer to this is like a stock market tip: It’s not about TIMING the market. It’s about time IN the market. In other words, you need to be looking at this as a long-term goal rather than thinking you’re going to lose 50 pounds in 2 weeks. In this case, a) you’ll need to get moving and doing exercise (see above comment regarding cardiac rehab); and b) I would strongly recommend visiting a registered dietitian and learning some ways you can improve your eating habits to put you on a slow and steady weight loss trajectory. Please do NOT go out and buy any infomercial products or miracle fat burning or metabolism booster supplements. The only thing you’ll lose is money and you’ll be stuck where you are.
The bottom line is that you need to get some good quality sound health information, get on the right track, and then remain consistent with it for the rest of your life. We’re not talking about “going on a diet” to lose weight and then drop it when you’ve reached your goal. We’re talking about overhauling your life. This can be an overwhelming experience so it must be done in a slow and gradual way. If you’re feeling very distressed about your health, I would also strongly recommend visiting a psychologist who has experience in health coaching and can help you create a systematic and stepwise plan to get your back on track. I’m not going to sit here and tell you it’s easy. There is no magic wand anyone can wave, but if you are prepared to finally say enough is enough, then it’s just about getting on track and staying the course. One day at a time..
Hope this helps. Best wishes to you
Kind regards,
Bill
Hi Dr Bill,
First of all thank you for posting up this really informative page, and for all your time & effort in replying to our questions. I’ve found it really reassuring.
I am a 42 year old woman from the UK who really enjoys an active lifestyle. Cholesterol/ weight / blood pressure all good (excellent really) and no family history. In April 2016 I ran my first half marathon and was looking forward to running further. Just a week later I started feeling (what I know now was) angina while running up hills, and although I could warm up into my runs fairly easily, the chest sensations continued during heavy exercise for a couple of weeks. After a visit to a fantastic GP and escalations I was diagnosed with a 70-80% blocked LAD and had a stent fitted in May. The procedure / recovery went well and my exercise tolerance test where they let me exercise to exhaustion was “excellent”.
Obviously I’m delighted to have been diagnosed and treated, but now, a few months on, I’m looking to the future and what I can/can’t do in terms of exercise. My cardiologist originally said that I could “now do any exercise that I wanted to do” but when I specifically asked if that meant I could run a marathon said no, I should probably limit myself to half an hour of running. He did say there was no evidence either way but that he would be concerned about dehydration on longer exercise sessions. I am now on atorvastatin, aspirin 75mg, clopidgrel, and dilzem (he first thought I had cardiac X syndrome and then decided to keep me on this one).
I have since been running (30 minutes / 5km at a time) and have taken up personal training with a medically-orientated trainer. I make sure I can talk all the way through my sessions and tend to watch my heart-rate and keep it around 140bpm or lower (I have no idea what my max heart rate is, unfortunately). I feel fantastic during exercise, and haven’t had any angina since the PCI.
My questions are – is it safe to do this? Is it safe to increase my run to an hour?
Is there a maximum sustained level of heart-rate that I should be aiming for, or is the ‘talk test’ OK?
Given that my cholesterol / blood pressure were already good do I need to modify my diet to reduce fat & salt?
Really, I guess I’m asking how many concessions I have to make!
Thanks in advance for any advice.
Catherine
Hi Catherine,
Thank you for your comment. You seem to be pretty level-headed about all this and that is a very healthy way to be. As I’m sure you can appreciate from my other comments on this article, I can’t provide any specific guidelines since I’m not familiar with your entire medical history, nor can I give any information that goes against your doc’s recommendations. BUT, I can provide you with some talking points you might which to discuss with him.
1) provided your PCI was completely normal with no complications, you’re young, you’ve got a history of exercise (including a marathon), then you might wish to plead your case again with your cardiologist. I’ve had some pretty serious cyclists in cardiac rehab, one guy of which had three heart attacks with significant damage to his heart muscle and diagnosed congestive heart failure. Despite all the things wrong with him, he kept on going out and riding his bike for hours and hours with no ill effects. But in his case, the rest of his body was quite fit so that it offset his very sick heart. In your case, you did not have a heart attack, so you do not have any compromised heart function (you had a plumbing problem rather than a heart problem).
2) Dehydration “could” plausibly be an issue but only if you were not drinking on a regular schedule during your marathon, or if the conditions were quite hot.
3) If you’re still taking Dilzem then this should slow down your heart rate a bit, making it unlikely that your HR is going to shoot up into the stratosphere. If you’re getting your heart rate up to 140 bpm, then that’s about 78% of your age-predicted max HR (but your actual max HR “could” be higher or lower if it was actually measured). Given your fitness level as you describe it, 140 bpm is not uncharted territory and is unlikely to pose a problem unless you happen to have other arteries plugged up.
4) Regarding duration, we frequently had patients in cardiac rehab exercising for an hour at a similar percentage of their age-predicted max HR. However, only your cardiologist can officially give the nod on that one.
5) The talk test is always a good standby aside from heart rate, so I think that’s always a good indicator of how you’re going with the intensity.
6) Regarding fat and salt, for specific info, I would recommend consulting a university-qualified dietitian to deal specifically with your diet, BUT, I will point out that salt tends to be an issue mainly in salt-sensitive people (not sure if this applies to you). Some people can eat salt by the bucket-load with no ill effects and other people can have a small amount and it bumps up their blood pressure. But that aside, in general, it’s never bad advice to keep salt intake at low to moderate levels as a safeguard. Regarding dietary fat, in and of itself, fat is not necessarily bad, but as with all things, too much of anything isn’t going to do you any good. I would defer to similar recommendations as with salt in that it’s never a bad idea to keep fat intakes at reasonable levels (approximately 30% fat or less and of that 30% less than 10% coming from saturated fat). Fat is a very energy-dense source of nutrition and has a lot of calories packed into a small amount (hence the reason it’s easy to overeat them).
The bottom line is that you may wish to speak to your cardiologist again and perhaps discuss having a treadmill stress test done. If you’re pushing yourself to max (or near max) and there is absolutely nothing out of the ordinary happening with your heart, then that at least gives you both reasonable confidence that your ticker is strong (and there are no odd blips on your ECG).
I would also advise you to pay extra special attention to any other signs or symptoms that may arise. Hopefully this was a one-time thing for you and you’ll never have it happen again. But if for any reason it does, at least you know the symptoms from your first episode. Quick treatment means no heart damage, and that’s very important when it comes to exercise capacity.
I hope this response gave you somethings to consider and things to discuss with your doc.
Kind regards,
Bill
Hi Catherine Your story is very similar to mine. I was 42, very sporty all my life, nothing ever in excess but still ended up with 2 stents in my RCA. Anyway I went and saw the leading sports cardiologist in the UK to get reassurance that I could continue my endurance sporting activities as pre MI. He put me through a thorough stress test, took my HR to 193 and confirmed there were no odd rhythms, also checked my heart function and ejection fraction as best they can with ECG which was all normal so there have been no restrictions applied to me apart from no events that subject you to electric shocks and ice pools ;-). If you want his details and it’s ok with Dr Sukala then I can share here or privately via mail
Hi Rav,
I’d be happy to approve the comment if you’d like to share your cardiologist’s details. Cheers, Bill
HI Bill
The Cardiologist’s name is Professor Sanjay Sharma.
kind regards
Hi Dr Bill,
Thank you so much for your reply and taking the time to advise me.
Sorry if I didn’t make it clear in my original post, but I did have a treadmill stress test, one month after the PCI (4 months ago). I did 15 minutes of the Bruce protocol and got my heart-rate up to 176bpm without any abnormalities on the ECG. Prior to the procedure I had been asked to stop the stress test early as my ECG on exercise was abnormal. Hopefully this is additional reassurance that things are now running smoothly.
Thanks also to Rav for his post about his similar situation. It’s good to know that I’m not alone! I’d be really interested to know of other people in this situation and whether it did turn out to be a one-time thing for them, or whether there were other narrowings later. My cardiologist suspected that I may have had a chest infection or something to trigger the lesion since he didn’t expect me to have significant atherosclerosis based on blood tests and lifestyle.
Thanks again for the advice
Catherine
Hi Dr Bill
I have been gym fanatic for since age of 18.Now iam 55.Recently i felt jaw pain during treadmill running and went to see my friend cardiologist who did ETT and stress echo Treadmill showed signs of RCA disease but stress echo was normal with no troponin leak. My TC was 4.1 with HDL of 1.06 and LDL of 2.2.On angiogram there was a very soft 94% occluded RCA which was stented and also mild LAD lesion with 60% lesion in diagonal artery.
My main issue had been stress for years with poor sleep which i guess has contributed to hypertension and CAD.Hypertension is very well controlled
Whats my prognosis?Can i play competitive sports like golf?Is athersclerosis reversible?
Iam only on aspirin , plavix(3-6 months) and ACE inhibitor
Hi Vijay,
Unfortunately, I can’t answer any of those questions since they’re pretty specific and are best answered by your cardiologist who’s most familiar with your individual medical history and circumstances. If you can get into a cardiac rehab that’ll be the best way to get back on track.
Hi Dr
I am 39 yrs old and regularly play golf every week and up until last November 2015 I was playing 5-a-side football and jogging for around 20 minutes once a fortnight. On 5th November I was playing 5-a-side football and had a pain in the very centre of my chest after 3 minutes running. I stopped and the pain went. This went on for some time every time I ran. Long story short I have just been into Leeds General Infirmary a week ago and a stent has been placed in my artery (MID LAD whatever that is?).
I want to know if I will be able to resume playing football and jogging. I have continued to play golf throughout all of this with no problems at all thankfully as it is my number one hobby. I am on asprin, atorvastatin, amlodipine, clopidogrel and bisoprolol and have been for a month (leading up to the angioplasty).
I have had a few strange twinges in my chest during the week following the procedure and had what felt like very mild angina when sat on couch but nothing for the last couple of days and it may just me being paranoid?
Can I start a slow jog now to test whether I get the pain again? It used to occur after just 2 or 3 minutes of jogging?
Thank you for your time and I am thankful I have found your page.
Dear Dr Bill Sukala, I am 55 years of age and had a heart attack back in 2005. As a result I had a stent (Texas?) fitted. My medication following this was: Plavix, Lipotor, Ezetrol. Following my Cardiologist’s advice a few years ago I stopped taking Plavix and take Cartia instead. I am also on Methotrexate, Arava and folic acid for Rheumatoid Arthritis (Psoriatic). I believe I am healthy, reasonably fit and have a good diet. Even before my heart attack I believe I was fit and diet was average. My Cholesterol at the time was about 6, now it is over 3. I slowly returned to what I believe was good fitness after starting boxing (for cardio) a few years ago. I now like it very much. Each boxing class starts out by doing rope skipping, learning boxing techniques followed by some light sparring and focus pad workouts. Recently I had a three round (3 min bouts) where we only could punch the body of the opponent. Soon I will be fighting in a full on three round fight – with of course head gear and mouth guard protection. I like learning the technical ability of boxing and will not be doing any further actual fighting in a ring once I compete in the bout above. After my first bout, I was very exhausted and somewhat bruised as well. My GP today said he would rather me play golf. I did check with my Cardiologist some time ago whether boxing was alright to do, and he said yes. But I wasn’t actually boxing in a ring against someone at that time. I do not see the Cardiologist anymore because he feels there was no further need as I was doing everything right and my blood tests and diet were stable. Could you please advise if doing one more three round / three minute fight be pushing my exercise and luck too much, and perhaps do more damage than good? Mainly concerned about being hit in the chest area. Thank you for your time.
Hi Kim,
Based on what you’ve provided, you had your heart attack and stent placement back in 2005. By now, your stent is fixed and is unlikely to go anywhere. As a general rule, being hit in the body is probably not a good thing, but based on my experience in cardiac rehab, I have not come across anyone who’s had any problems boxing after an angioplasty provided they gave it ample time to health and settle in. In your case, you’re 11 years post-op, so that’s good. BUT, as a rule, I always tell people to speak to the cardiologist or the cardiologist’s practice nurse (ring the office) to see what they think. Unfortunately, I cannot give you any specific medical advice, but I’m hopeful this information is helpful.
Kind regards,
Bill
Hi Dr Bill
Sir i am 29years old guy. I recently had angioplasty n a stent in LAD with 100percent blockage. I was very active guy and used to walk alot. It was shocking for me and for everyone in family that this all happened to me. I am taking all my medicines on time. Quit smoking. I am 6ft tall n weigh around 72kg. Doing light exercises as well. Sir i would like to know, am i going on the right track? Will it happen to me again? Can i live normal life or is it me thinking i am abnormal now??? Please help, i lack motivation in my life nowards.
Hi Rahul,
I can imagine this would have come as a massive surprise to you, but it does not mean that it’s the end of the world. If you feel a bit anxious then that is quite normal and expected. If you are making the lifestyle changes such as quitting smoking, that will help you minimise your risk of having another heart attack. The good news is that, based on what you wrote, you did not have a heart attack. So this means you did not have a “heart problem” but instead you had a plumbing problem in one of the arteries that feed blood to your heart (like a clogged pipe). You’re much better off if you did NOT have a heart attack because this can cause heart muscle damage. Consider yourself lucky. I would recommend participating in a cardiac rehabilitation program (if there is one at your hospital) and also visiting a dietitian with a degree in nutrition. That will help you safely exercise and receive reputable information on what to eat to keep healthy for the long haul. If you have a lot of ongoing anxiety, I would strongly recommend visiting a counsellor with experience in working with people who have had medical issues. It’s a sign of strength to reach out for help, not weakness.
Hope this helps,
Bill
Hello Dr Bill,
I have found the information in the letters above to be extremely informative. Thank you for that.
6 weeks ago I returned from a bike ride (35km and building my fitness through running riding, squash, basketball and touch football to attempt a mountain race consisting of kayaking, running and riding). I suffered chest pain after the ride and my wife drove me to hospital. On the way I suffered a heart attack. In hospital I went into Cardiac arrest and was revived. (3 to 4 minutes down). I was transported by helicopter to a larger hospital and again suffered a heart attack during transport. On arrival at the hospital I was fitted with a stent LAD with 60%mid lesion.
8 days later I was fitted with 2 more stents, mid LAD 80% lesion, and mid right PDA 80% lesion. An echocardiogram showed an EF of 45 to 50%. My troponin reading on the day of the CA was 92888.
All in all I am a very lucky 57 year old male to be questioning you today thank you to the prompt intervention of the hospital staff. By the way , I am a fit, nonsmoking,light drinking, BMI 23.5, active person.
My question is – over time do you think it will be possible to regain my former fitness levels? Play touch and squash? Climb Mt Kiliminjaro? Etc
Your advice would be much appreciated.
Also, I am doing cardio rehab but find it a little slow. Do you think it would be worthwhile to approach physiotherapists to design a specific program for rehabilitation, or what other approach would you suggest?
Again your advice would be much appreciated.
Last year I had a prostatectomy and recovered my fitness and mind set quite quickly after that.
Regards
Greg
Hi Greg,
Thanks for your comment. I’m glad to see that you’re attending a cardiac rehab program so I would encourage you to take full advantage of what’s on offer while there. I know that you’re a fit guy going into this, but sometimes fit people are also difficult patients! I know because I’m one of them! The fact that you’ve had the heart attack and probably a bit of mild cardiac damage (given your ejection fraction) means that you’re going to need to make sure you’re healed and you’ve got the all-clear from your cardiologist before you go back to doing things full throttle.
I would suggest having a heart to heart talk with your cardiologist (no pun intended) and discuss having a max treadmill stress test before you get back to flogging yourself. This will let you know that your heart is functioning well and you are not having any funky changes on the electrocardiogram (arrhythmias) which might preclude you from doing higher intensity exercise. Your doc can discuss all the pros and cons of the test and what it will and will not tell you. But as an exercise physiologist with experience in cardiac rehab, a treadmill test will at least help you minimise risk. If you’re stable at high intensities during the test then with reasonable confidence, you should be able to handle higher workloads out on your own.
If you’re still attending cardiac rehab now, I would ask them if they can put you on a telemetry monitoring system whilst exercising. Even if not doing max intensities, it will let them know if you have any arrhythmias during exercise (benign or otherwise). In my experience, we always put the post-heart attack people on telemetry for several sessions to ensure they were “Stable Abel.”
Regarding a physio for a private program, many of them are good at muscles and bones but don’t have a lot of knowledge or experience with cardiac patients. Some do, but many don’t get much training in that regard. A better bet would be to find a clinical exercise physiologist with specific training in working with clients with cardiac issues. Send me an email through my contact page if you need further assistance.
Kind regards,
Bill
Hi Again Dr Bill,
Thank you for your informative and detailed reply. There are certainly many things there which I will take on board.
Unfortunately, as I live in a country town(Grafton) the availability of Telemetry equipment is questionable, but I will check.
One more question if I could? Do you know any exercise physiologists within a couple of hours from Grafton that have cardio rehab experience? I don’t believe there are any locally.
Thanks again for your support and help.
Regards
Greg Eather
Regards from GREG and his
Thank you again for both your time and advice. I have emailed Dr Broadbent.
Regards
Greg
Hi Bill, thanks for your article. I realise I am jumping the gun on this one, as I am having an angiogram in 2 days time and don’t yet know whether an angioplasty will be necessary. I am a 66 year old woman and have not had any heart attacks. Up until now my issues with my heart have only been the rhythm. 12 years ago my heart suddenly started beating slowly and intermittently stopped beating altogether, as a result I now have a pacemaker. Since then I have had one episode where my heart was consistently beating too fast but a change of medication (from Atenolol to Bispronol) seemed to fix that. However, I then started getting some episodes of atrial fibrillation and subsequently some atrial flutter. I did have an ablation procedure a couple of years ago. My Dad died in 1976 at the age of 58 so since then I have made a point of following a healthy lifestyle (he didn’t) including a lot of exercise, more so now I have retired from work and have more time. I gave up competitive running in my 50s but still kayak, cross-country ski, swim laps and hike. So much for the background, now for my question. If I do have to have an angioplasty, can I travel a week later? I booked a small group tour in Costa Rica with a friend which I am reluctant to cancel unless absolutely necessary. There will be opportunities to do some longer, possibly steeper hikes there but these are optional. My concern is mostly around carrying luggage from place to place as I read that heavy lifting is not good. And I will be flying there and back if I go.
I will of course follow my cardiologist’s directions if I have the procedure, but I would be interested in hearing your opinion. Most of the comments on your page are related to fast and competitive sports but I have always been one for endurance rather than speed.
Thank you for your assistance,
Elaine
Hi Elaine,
Sorry for the delay in responding. Your comment ended up in the comment sin bin for some reason. I saved it and am now responding!
You mentioned you have an upcoming angiogram and are not yet sure if an angioplasty will be necessary. I think first and foremost, you’ll have to take it as it comes. If they perform an angioplasty with or without a stent, obviously the recovery will be a little bit different. As you pointed out, your cardiologist’s advice is the final word since the doc is going to be most familiar with your medical history. I would suggest discussing your intentions for Costa Rica with your doc and get specific guidelines that are relevant to you.
Speaking from an exercise physiologist’s point of view, provided your angiogram/angioplasty/stent and recovery are all normal with no unforeseen complications, and you’re approved for activities by your cardiologist, then I can’t imagine doing activities of daily living will pose much of a health risk. If you’re lifting baggage but are not struggling and turning red-faced in the process, you should be ok. I think if you’re lifting really heavy bags and are grunting and groaning, then that’s a different story.
I think one of the things that people tend to forget is that routine surgery is still surgery and there is still healing happening on the inside (and perhaps at the catheter insertion site presumably at the femoral artery). For all normal light lifting, you should be ok, but it’s still prudent to ask one of the young stallions in your group tour if they can do the heavy lifting for you (as required) until you’re fully healed.
Again, I need to be clear, I am not providing medical advice or giving you information that is a substitute for that of your cardiologist. Discuss your concerns with your doc and I think you’ll get the answers you seek that are specific to your situation.
Hope this helps,
Bill
Dear Dr.Sukala
I follow you as runner from Turkey.I am 52 years old male. I had a heart spasm last week and they placed a stent .I run 10-15 km. everyday for 10 years.I also run marathons.I am very dissapointed and I dont want to quit running.I am waiting for your advices and a program that is suitable for me. Thanks
Ozgur Kosar
Hi Ozgur,
Thank you for your comment. First off, you are still in a recovery phase so you still have some healing occurring inside your heart. You should discuss your recovery plan with your cardiologist who will be most familiar with your complete medical history. If there is a cardiac rehabilitation program available to you, I would also recommend participating in it so you can exercise under supervised conditions to ensure you transition smoothly back into your training program.
I do not provide full exercise programs over the internet, as this would be negligent on my part for not knowing your entire medical history. I would recommend you speak to your cardiologist to discuss having a treadmill stress test (after you’ve healed) to ensure that your heart is stable and there are no signs or symptoms (or changes on the electrocardiogram) that could pose a problem.
If you can find an exercise physiologist or personal trainer with experience working with cardiac clients, then they can help you there in person to transition you back into your running routine. Hope this helps.
Kind regards,
Bill
Hi
I’m 63, female and had 2 drug-eluting stents fitted a couple of days ago. My angina symptoms were in my jaw and between shoulder blades and for over 2 years had been put down to my arthritis by my rheumatologist! I was taken into hospital with severe pain and diagnosed with unstable angina. There are no vacancies at rehab at the moment but I will go once called. I’m limited in what I can do due to arthritis but thought I would begin with gentle walking. I’m really not fit and wondered how long I should walk for. I must admit I’m worried about having another angina attack if I overdo it. Or is there something else you can suggest? I aim to go back to work after a week, although only part-time for the first couple of weeks.
Hi Jennifer,
Thank you very much for taking the time to leave a comment. While I’m not happy to hear you had angina (ouch!), I am happy to learn that you were able to get a proper diagnosis and treatment. If you have a documented history of other aches and pains, then it’s not uncommon for these sorts of things to be chalked up to arthritis pain. I’ve seen it before on a number of occasions. But onto the here and now, let’s see if we can get you on the right path.
Here’s some good news. Based on the info you’ve provided, it looks like you only had a plumbing problem (the arteries) as opposed to a heart problem. If you have a heart attack with damage to your heart muscle, then that is an entirely different landscape from a recovery standpoint. So hopefully that helps put you at ease.
Remember that you’re still pretty fresh out of surgery and there IS still healing happening on the inside. Even if you feel well, remember not to push it too hard (as I mentioned in my article). The key is to keep your heart rate and blood pressure from climbing too high while your stents are settling in.
Regarding cardiac rehab, I strongly support your participation in a guided program once a spot opens up. It will give you a lot of peace of mind and will allow you to sound off to the cardiac rehab staff regarding any questions or concerns that are specific to your individual situation.
As for what you can do in the meantime, I would suggest speaking to your cardiologist and/or the practice nurse at the clinic to ensure that you’re medically stable (i.e., no medical reasons which would preclude you from safely walking around your neighbourhood on your own). Provided they deem you stable and low risk, then going out for walks as I’ve outlined in my article would be very helpful in getting you back on track and feeling strong again.
Regarding another angina attack, if the docs were able to treat all affected arteries, then it’s unlikely you’ll have angina again (and assuming the two stents they put in were a success). You do need to be aware of how you’re feeling while walking. It’s not uncommon to be a little bit leery getting back into it, always fearful of the angina setting in again.
As for going back to work, depending on what kind of work you’re doing, perhaps it’s best to speak with your doc and get approval. If it’s desk work, then probably no issue, but if anything physical that requires any lifting or exertion, then maybe best to check just for good measure.
Hope this helps.
Kind regards, Bill
Hi Dr. Sukala,
I had angioplasty and a bio absorb stent placed in my LAD 5 1/2 weeks ago. I did not have a heart attack so I have no heart damage. Last spring and halfway through the summer I was able to be very active. I ran a couple of half marathons and in July did a short triathlon. Around August I was unable to do cardio anymore because of chest pain, however, I continued to lift weights up until the stent was placed. I am now back to doing cardio and just this week I started lifting light weights again. Right now I can do from 20-40 minutes of cardio at a time depending upon intensity.
I live in Nebraska and it gets cold in the winter. I have been told that I shouldn’t shovel snow this winter and I shouldn’t run outside this winter. But do you think I can go ahead and shovel some light snow and do some easy outside runs if I wear a face mask and don’t overdo it? Also, if you think that is a possibility is there a particular kind of mask you would recommend?
Thanks,
Hi Jim,
It sounds like you’re on track regarding your recovery. For the first month or two, it’s true you’ll need to be more cautious. There are general recommendations but individual recovery can vary from person to person slightly depending on their condition, how complicated the surgery was, pre-surgery level of fitness, etc. The main reason they tell you not to shovel show is that it can get heavy and jack up your blood pressure. While you’re in recovery, this can be an issue so they generally tell people not to overdo it (particularly if the snow is wet/soggy snow). If you’re nearly 6 weeks post op, you’re medically stable, and you’re already doing 20 to 40 minutes of cardio, then this is a good sign that you’re on the right path. I would recommend you speak to your doc about resistance training and, if given the green light, then ask if shovelling light snow would be an issue. As I’m sure you can appreciate, I can’t give any specific advice since I don’t know each commenter’s full medical history. Hope this helps give you some direction though. Cheers, Bill
Hi Doc
I an 55 years old male, I had 3 stents put in 6 months ago, no issues with the op
But I get a bit of pain when I lay on my left side, when I go to bed, or when I raise my left are above my head when laying down, or when I am just sitting still watching TV
I do not get an pain when I am active/ working, is this normal?
Cheers
Steve
Hi Steven,
Hard to say exactly what’s causing this, but I would recommend discussing it with your cardiologist or practice nurse. I’ve heard of this in other people as well but can’t say for certain it’s cause and effect or coincidence. Feel free to stop back here and post another comment after you speak to your doc, so others might benefit from this information as well. Kind regards,Bill
I had a stent placed on 21st of December. I have just been released to full activity !!!! I am 61 in good shape and an avid cyclist. I ride 150 miles a week before the stent. I ride with a group and we ride training rides in an ” A ” group pace (30 miles we will finish at 19.2avg mph) , My question is I am taking Brilinta 2 times a day with 1 aspirin. My PCP doctor is scared taking that much if I fall I could bleed out if I landed on my head ? when can I cut back on the thinners so I can ride ?
Hi Ken,
Thank you for your comment. You certainly sound like a very fit person. Provided you did not have a heart attack and only had a stent placed, then this means that you only had a “plumbing problem” rather than a heart problem (i.e., heart muscle damage). It might be worth discussing with your cardiologist the possibility of having a treadmill (or cycling) stress test done to see how your ticker and hemodynamics are after the stent placement. I often tell athletes like yourself to discuss this with their docs since you are pushing the higher intensities. It will give you some peace of mind.
As for Brilinta and aspirin, yes, they are blood thinners and there is an elevated bleed risk if you fall. That is true. I would discuss the risks versus benefits with your doc. You’re 61. How many years have you been a cyclist and how many nasty falls have you had where you banged your head? You seem to be a well-trained athlete so I’d imagine you’re not in the habit of falling off your bike every ride. If you are cycling with a group, then if, God forbid, you did fall and bang your head, you’d at least have people there who could attend to you on the spot, as opposed to cycling on your own and ending up face down on the side of the road. Lots of factors and meta-factors worth considering and discussing with your cardiologist.
I can’t tell you when you can cut back on your thinners since I am qualified as an exercise physiologist and not a cardiologist. Moreover, even if I was a cardiologist, I still couldn’t provide you with any medical advice since you’re not my patient and I’m not familiar with your entire medical history. But definitely a question worth discussing with your doc just the same. Hope this information was helpful for you.
Kind regards,
Bill
Hi Bill
Thank you again for your 2 previous replies to my questions.
I did try and email Dr Broadfoot, sp? but at this stage I have had no reply. Ian still looking for an exercise physiologist that has telemetry equipment as close to Grafton as possible. Possibly somewhere in the Gold Coast ?
Any suggestions?
I am to do a nuclear stress test on March 2nd, so hopefully this will give me more direction.
One last question. Does your clinic, assuming you have one, work on exercise physiology with telemetry equipment and do you or some else see patients?
Regards
Greg Eather
Hi Greg,
Thanks for getting back to me. Dr Broadbent has just recently taken up a position at University of Sunshine Coast so is no longer at SCU (which would explain why she’s been hard to reach!). Nevertheless, the telemetry equipment is still available at SCU and you can try to set something up through a colleague of mine Sonja Coetzee. Here email and phone number are listed there.
I’m not too sure about who on the Gold Coast is doing training and testing with telemetry, but you can get in touch with Jack at Making Strides in Burleigh Heads and he might know who is doing that sort of thing there (info {at} makingstrides.com.au 07 5520 0036).
I have telemetry equipment here in Sydney but am working on private consulting contracts at the moment so am not currently seeing new patients. However, if that changes and you’re in Sydney, I’d be happy to see you here at that time. But best bet for now would be to contact Sonja and see if they can get you into the SCU clinic.
Cheers,
Bill
Thank you so much Dr. Bill for this article. It was very informative.
I was searching for some guidelines to help my fiancee who had a major attack in Oct2016, & 1drug eluting stent implanted. The cause, as mentioned in the report is the rise of homocysteine level.
Thank you, once again 🙂
Thank you Dr. Bill for providing such wonderful information!
Hello Dr Bill, I found your article very helpful and reassuring. I just had a stent placed six days ago following sudden chest pain, which turned out to be a small heart attack.
I am 63 and very fit for my age, as commented upon by paramedics and doctors in the last couple of weeks. I run, cycle, do some weights, bench work regularly and have always felt great. My resting heart rate is very slow, which apparently was a good thing.
To add to this, last Christmas I took early retirement from teaching and now add gardening to my pastimes. Overall I have increased my physical activities and have felt great, so this event has really dented my confidence. I did get a warning when on my bike a couple of days before the attack, I had a similar pain, but it subsided, was going to follow up at the docs, but didn’t. I think when you are normally fit and healthy it is maybe difficult to spot the signs that should be looked at seriously. They may in the end be nothing, but worth checking out.
My consultant told me that my arteries were in great shape, all smooth, just this one block, now fixed with a stent. There has been no mention of muscle damage, and I left hospital the same day stent was placed. I have a cocktail of drugs, asprin, clopidogrel, ramipril and atorvastatin and see the GP on Friday where I hope to find out more about these drugs and my general condition. I do feel almost like I did before, but am now pre-occupied with every ache and pain concerned that maybe there’s a new or recurring problem. Just looking to getting back into an exercise routine and doing things like mowing the lawn, which is taking advantage of my inactivity!
I needed some reassurance that this isn’t the beginning of the end, and that I can return to normal activities eventually, so your article was very helpful in providing that hope. I find this all difficult to take in not having any history of heart or any other problems. Also going from someone who never takes medication to a lifetime daily does is hard to accept.
When I get my head round all this I hope to adjust my thinking and then move forward positively. Thanks.
Hi Tom, Thanks for taking the time to leave a detailed comment. First and foremost, based on everything you’ve mentioned, you appear to be very aware and interested in taking good care of yourself. THAT is extremely important. There are many people out there smoking cigarettes, eating cheeseburgers, and doing no exercise who go through the same thing you did, but then have no intention of improving their lifestyles. So on that note, you are well ahead of the curve. In my experience from having worked with countless cardiac rehab patients, it’s pretty uncommon to just drop over from a heart attack. Most people have signs and symptoms but whether they choose to act on them (i.e., get medical attention) is what makes the difference. In your case, you took action and, despite the fact, you might have had a small heart attack, the good news is that you did not have any heart muscle damage.
As for medications, the meds you’re on are commonly prescribed after an angioplasty/stent. I would suggest you speak to your cardiologist about the possibility of either reducing dosages over time or, best case scenario, discontinuing them if/when appropriate. I’m a clinical exercise physiologist so obviously I can’t tell you what to do, but definitely worth having a talk with your doc about your specific situation.
Bottom line is that this is NOT the beginning of the end. I have worked with a lot of patients who succumb to “illness mentality” where they let it infect every thought they have and it limits their ability to enjoy their lives. It’s what we call “learned helplessness” (i.e., “oh, I can’t exercise because I have this heart condition…”). You have some choices to make from here on out and that is, how do you want to live your life? Choose that first and then determine how you’re going to make that happen. I’ve seen a LOT of patients go on to live fully vibrant lives, running marathons, surfing big waves, etc. It’s quite normal to have a bit of anxiety after a heart attack/angioplasty/stent. If you feel this is a factor for you, I would strongly suggest speaking to either a psychologist associated with the hospital where you were treated. They are VERY familiar with the changes that people go through when it comes to medical issues. You are not alone and reaching out for help is NOT a sign of weakness. Quite the contrary, it is a sign of strength. Overall, I would say that it’s important to be insightful and reflective of the thoughts and feelings you’re having and ask yourself if you’re having thoughts that might potentially sabotage you’re physical and mental well-being. In closing, rest assured that it’s normal to have to adjust to all this, but you will be ok. Feel free to stop back and leave an update so others might benefit from your experience. Kind regards, Bill
Dear Doctor
I underwent PTCA on 19th April 2017
Reduced weight by 5 kg
I am a good swimmer.
Could i start to slow swim in swimming pool ?
I also do deep breathing and Pranayama as per indian tradition.
Hi Sadashiv, Thanks for your comment. I would suggest speaking to your doctor first to make sure you’re medically stable. If the doctor gives you clearance to start swimming, you should be fine. Just pay attention to your heart rate and blood pressure and ask your doctor what would be acceptable limits for each of these. Hope this helps. Kind regards, Bill
Hi Doctor Sukala,
I did martial arts for the beast part of 30 years, retiring from the sport back in 2005 due to arthritis issues restricting my activities (I am now 64)… In Feb of 2013 I had a stent inserted in the “L.A.D.” artery. There was also damage to other arteries but only one stent was inserted. Since then, while doing very little exercise, I get extremely hot very quickly. For example, a group of us get rugged up to go quad bike riding along rough bush tracks in winter. I am the only one to get so hot and sweaty even on cold days. The same if I do any work around the house. I don’t seam to notice as much on warm or hot days, just in cold weather. Could this be a side affect of my medication? My cardio guy couldn’t really explain why. I am taking Coplavic, Perindopril, Metoprolol, & Atorvastatin for my condition.
Thanks, Regards,
Jim
Hi Jim,
Thanks for your comment. It’s tough to say for certain what’s causing your increase in sweating, but I don’t think it’s beyond the realm of possibility that one of your meds could be the culprit. Everyone’s constitution is a bit different but, if it helps confirm you’re not crazy, I have seen this with other patients in cardiac rehab. Specifically, a lot of people complain that the beta-blocker (metoprolol in this case), which lowers heart rate, makes them feel a bit sluggish. That said, they feel like they have to exert themselves more to do things that previously felt easier without the med. But then I’ve had other people say it really didn’t drag them down too much. You’re also on a blood thinner (Coplavix), ACE inhibitor (Perindopril) and a statin (Atorvastatin), all of which would have their own individual potential for side effects.
Having said that, I often recommend people sit down with their cardiologist and level with them saying something to the effect of, “listen, I’m having side effects which I think are being caused by the meds (or perhaps interactions between them) and it’s impinging on my quality of life. Can we try something else that might be a bit friendlier to my system?” Your cardiologist is going to be most familiar with your medical history so is best qualified to help you find a medication that’s right for you. You might also ask if it’s appropriate to lower your doses a bit, depending on your blood pressure and other factors.
Hope this helps.
Kind regards,
Bill
Hi Dr.
Thank you for an informative article.
I am 55 years old been a fitness fanatic all my life and a serious gym bunny for 20 years. On 3rd April at 6am in the gym I felt massive pain in my chest and down my left arm, rushed to hospital and low and behold 2 stents later. I am yearning to get back into the gym again (Not been since 3rd April) would like to get into my weight training again (Missing the endorphins) The procedure seems to have affected my Psychologically as I am petrified to go back…. Is this normal?
Thanking you in advance.
Regards
Pierre
Hi Pierre,
Anxiety is a quite a common occurrence after chest pain (or a heart attack). I would suggest speaking to your doctor for a referral to a hospital psychologist or social worker that specialises in helping people after a medical event. Exercise can be a scary proposition after angioplasty/stent, but provided you are medically stable and your doctor has given you the all-clear, you should be able to start easing back into your exercise routine. If you’re able to enrol in a cardiac rehabilitation program, the staff could help you establish safe exercise guidelines around heart rate and blood pressure. Hope this helps. Kind regards, Bill
Hello doctor
My husband aged 44 had a routine health check up on 25 th apr 17 for insurance policy,got high cholesterol…went for tmt ,got positive on that ,went for angiography ,found multiple blockages in all vessels.he had 0 symptoms at tge time of test. On 25 th may,he had 3 stents placed as an intervention ,2 in rca and 1 in lad.now he is home resting with a plethora of medication.
He was walking on treadmill everyday for 30 min at 6-6.5 km per hr speed and various inclines.he was also into biking occasionally upto 10 km distance. He was a smoker till 2009 and quit since then.he enjoys his scotch on weekends 3-4 drinks.now dr has asked him to take it easy for 2 wk( walking 5-10 min 3-4 times a day) then slowly build.
I would like to get ur advice on how he should carry on after 2 wk which will be over by 7 jun.also can u pls suggest abt alcohol intake.he is 5’10’ 81 kg 44 yo indian male.non diabetic.there are other minor lesions as wel which are unstented .
Hi Swati,
Thank you for taking the time to leave a comment. Your husband is very lucky that they found the blockages before it caused a heart attack. On that note, he did not have a “heart problem” per se. He had a “plumbing problem.” His heart muscle is still normal and does not have any damage so he is very fortunate.
While I cannot legally give any specific advice since that is the role of his cardiologist, I’ll say that the first couple weeks are going to be very important due to healing happening around his stents inside his coronary arteries. He should still be up on his feet and moving around so he doesn’t get stiff. As I pointed out in my article, there’s nothing wrong with doing his activities of daily living, but he must be careful not to do any strenuous activities which might increase his blood pressure and heart rate.
After two weeks, he may continue to gradually build up his exercise duration from 5-10 minutes to longer durations but for fewer times per day, eventually doing one long continuous exercise session.
As for alcohol, I would strongly suggest discussing this with his doctor, especially now that he is taking medications which may interact with alcohol. I’m not suggesting that he stop drinking forever, but for right here and now, he needs to accept that there will be some lifestyle changes he’ll need to consider.
Regarding his other lesions, find out what percent blockage the lesions are. Anything above 70% is usually when the docs make a decision to intervene. Your husband will need to keep aware of any signs and symptoms he might experience and seek medical attention immediately if he does experience symptoms (i.e., chest tightness, pain or discomfort in his left jaw radiating down his left arm).
Honestly, I would suggest he take the time to speak with a university-qualified clinical dietitian to help him with his eating and perhaps a clinical exercise physiologist to help him with his exercise. If he is experiencing any anxiety about all this (which is common), then there is nothing wrong with speaking to a counsellor through the hospital who is experienced helping people through medical events.
Right now, his best bet is to lead a healthy lifestyle and be patient through the recovery. Feel free to write if you have any further questions.
Kind regards
Bill
dear doctor Bill
i had earlier also taken advice from you regarding my husbands stent implants and activity post that. Once again i am here to bother you.My husband (now 46) was experiencing some discomfort in exercising (mostly treadmill) after 5-10 min of activity so we got him checked where after performing angio ,one more 90% blockage was found in LCX (this was 50% at the time of 2017 PTCI) and stented. Doctor also informed that one of his older stents in LAD also shows some plaque buildup but he could not assess the criticality of it. now my husband is home and resting. we have been told to resume walking slowly and build up over time. however my concern is the other blockage in older stent. what kind of exercising regime should he follow now and what should he watch out for.Also if you can help me understand why,despite all lifestyle modifications and all kinds of medications,he developed this blockage again.i am desperate to find alternate means which can help prevent this plaque development.in case you have come across anything for that in your extensive experience, pls. do share. Thanks in advance.
Hi Swati, Thanks for your comment. The best thing your husband can do is to 1) work closely with the cardiologists who will be most informed about his health; and 2) pay close attention to any signs or symptoms like you described earlier (i.e., chest pain, shortness of breath, etc). If the older stent has a little bit of plaque build-up, this does not mean it’s blocked. In general, it’s possible to have approximately a 70% blockage and not have any symptoms, sometimes more if the person has lots of collateral circulation around blockages (note: collateral circulation can occur in people who regularly exercise where their fitness masks their blocked arteries and they do not have symptoms). It’s also important to ensure he is eating well, mostly plant-based, mediterranean style way of eating. I would recommend seeing a university-qualified dietitian who may be able to help you with the diet side of things. As he starts feeling better after his recent surgery, make sure he remains active as this will be protective for his cardiac health. Kind regards, Bill
Hi Dr.
I’m hoping I can get some feedback on questions I seem to get mixed results from within my local medical community including my cardiologist, my cardiac interventionist, and my primary care physician. I’m a 50 year old male who has been in excellent shape my entire life but also had a 100% blockage (with excellent collateral artery growth thereby saving me from a heart attack) and a drug eluting stent installed 3 months ago. Prior to stent I was a power lifter and competitive athlete in racquet sports and basketball.
Through a watchful eye during cardiac rehab I was given clearance to return to an aerobic activity. Although never much a runner, I have been able to run 40-60 minutes with no harmful effects and the physicians are all pleased with that type of exercise. I can also report that I have generally been responding well to Plavix, aspirin and Beta Blocker as at rest heart rate and BP are exceptionally low.
The advice I get mixed results on relate to weight lifting and competitive sports. Some say go back to life you led before with no restrictions. Others express concern that the types of blood demand you place on the heart during heavy lifting is not advisable post any stent surgery. Same with particularly competitive sports that involve sudden, violent muscle movements.
For better or worse, I have gone back to a modified lifting program (never lifting more than body weight) as well as league play in competitive sports programs I still participate in. However, I’m frequently worried that although enjoying gaining my life back, I may be doing more harm than good for my heart and stent installed only 12 weeks ago.
Any feedback on dangers of weight lifting and or competitive sports participation (distinguishing from categorizing as recreational!)
Hi James,
Thank you for taking the time to leave a comment. There are a few concerns to bear in mind here.
1) Recovery time: you are now three months post-angioplasty/stent and I would presume that you have been back to your doctor and been given the all-clear to get back to exercise. Has your doctor performed a treadmill stress test to exhaustion? If not, you might want to discuss this with him and see if he/she deems it appropriate. If your angioplasty/stent is still patent and the doctors deem there to be no risk of the stent collapsing, then you would be a more appropriate candidate for higher intensity exercise (with clearance).
2) Other blockages? In this case, based on what you’ve written, it appears you had a blockage in one artery (but not sure which one). I would suggest speaking to your doctor to find out if there are any other lesions in any other arteries and, if so, what percent occlusion is present? Generally, docs tend to intervene when a lesion is around 70% or more. If you have other lesions which were not treated at that time, then this could plausibly play into whether or not the docs give you clearance for heavy lifting.
3) Intensity: If you were previously lifting heavy and your technique is quite good, then you’d be a much better candidate to resume your training regimen, provided that you have had a treadmill stress test and are cleared to perform heavy lifting (yes, they’re different, but at the highest intensities, the docs would be able to see if it induces any abnormalities in your rate, rhythm, or ST segment). I would be less likely to recommend someone BEGIN powerlifting for the first time in their life AFTER having an angioplasty/stent.
Hope this helps
Hello Doctor Sukala,
I am 42 years old and I had a heart attack 5 months ago due to 100% blockage of my Right Coronary Artery. I had an angioplasty and a medicated stent put in. I had no heart damage according to the echo. I was previously on testosterone replacement therapy for almost 8 years. My cardiologist took me off the testosterone because he said it can cause blood clots. Since then, I exercise daily and I have been on a low sodium diet. My testosterone is very low. I have no libido and I went from shaving my face daily to every 3 days. My cardiologist stated it might come back with diet and exercise, which it has not. What is your opinion on taking TRT with a stent?
Thank you, John
Hi John,
Thank you very much for taking the time to leave a comment. You mentioned you started on testosterone replacement surgery when you were about 34. Was this prescribed by an endocrinologist? The reason I ask is that there are a lot of “anti-aging” doctors out there who are very quick to prescribe TRT to men who might have technically “low” but not necessarily abnormal testosterone levels. And when it comes to tinkering with hormones and prescribing something like testosterone replacement therapy, there can be downstream issues if it’s not cautiously prescribed and carefully monitored on an ongoing basis.
As for the link between testosterone replacement therapy and coronary artery disease/heart attacks, the research isn’t conclusive at this stage. Here’s a link to a Mayo Clinic article which has a short write-up:
https://www.mayoclinic.org/healthy-lifestyle/mens-health/expert-answers/testosterone-therapy-side-effects/faq-20090015?reDate=28032019
Moving forward, perhaps it might be in your interest to speak to your endocrinologist (if you have one) or get a referral to an endocrinologist if you don’t have one. If you can have your endocrinologist and cardiologist work together, perhaps they can come up with a solution that will adequately address both your testosterone levels and your heart issues. I hope this helps.
Kind regards
Hi Dr Bill Sukala,
My name is Sonu. 9 months ago, I had a heart attack. I had one blockage which was addressed with angioplasty. Unfortunately I’m just 26yrs old now and I’m on medication for life. My medicines are:
-Morning: prasita 10mg / prolomet r25
-Afternoon: ecosprin 150mg
-Night: rosuvastatin 20mg
These are the medications I’m taking on a daily basis.
I just wanted to ask you, is it possible to go to the gym? If yes, then how much weight i can lift. I also wanted to tell you that my stress test and my treadmill were both excellent.
Please help me with the weight and also how often I can eat burger and stuff.
My last would be, is it possible for me to live my full life ?
Hi Sonu,
Thanks for your comment. While you are definitely young, the good news is that you performed well on your treadmill stress test. I would suggest you ask your doctor how much damage, if any, you had to your heart muscle. If you had damage, are there any wall motion abnormalities in your heart at rest and with exercise? If no damage, then your heart muscle should be functioning normally and exercise should not pose any significant risks (provided you have been cleared by your doctor).
Can you go to the gym and lift weights after a heart attack and angioplasty? While weight lifting should not pose any risk if you’re medically stable, I would recommend you speak to your doctor and get his/her final clearance to be on the safe side. No one should ever give you a definitive answer on the internet without being fully familiar with your entire medical history.
As for eating burgers, I would suggest increasing your intake of fruits and veggies more than anything since they are known to have numerous health benefits, some of which can protect the heart. If you have a registered clinical dietitian at your hospital, it would be worth getting a referral to discuss your diet in detail.
Can you life a full life after a heart attack/angioplasty? You absolutely can. If you are medically stable and well-managed, then you should be able to live a full and active life. If you ever have symptoms again, the most important factor is getting to the hospital as quickly as possible. In the cardiac rehabilitation world, we say that “time is heart muscle.” I am hopeful you will not have any more cardiac problems, but if you do, be sure not to ignore any signs or symptoms. The sooner you get treatment the less likely you are to have damage to your heart muscle.
Hope this was helpful.
Kind regards
Bill
Hello my father had “stent for narrowed arteries” three weeks ago. He is 56 years old. When is hot weather he coughs, have dry throat, he can’t sleep well, when weather cools down everyhing is alright.
The doctor who had installed stent told my father that he don’t have worry a thing. That he can do everything that he does every day, no prescription what to eat and what not to eat, should he drink coffee or alcohol nothing at all.
My father feels little bit dizzy, sometimes he blush. I don’t know what to do if he gets sick.
Hi Milan,
Thanks for your comment. I would first off suggest that you work closely with your father’s doctor to discuss these concerns. If the weather is hot and dry, then this can make just about anyone cough, not just someone who has had an angioplasty/stent.
If he is feeling dizzy, I would first recommend bringing this to his doctor’s attention to ensure it isn’t anything more serious. If he is taking medications after his surgery, then this can sometimes lead to drops in his blood pressure which could possibly explain why he’s feeling dizzy. If it is very hot and dry outside, then it is not uncommon to be a bit dehydrated which would reduce his blood volume and possibly cause his blood pressure go a bit lower than usual (plus any medication he’s prescribed which might also be contributing to his lower blood pressure). In this case, drinking adequate fluids will help maintain his blood pressure. But as I said above, my first and most important recommendation is that he speak to his doctor and work closely with him to address any concerns he might have regarding his blood pressure.
Kind regards
Bill
Sir please reply.
My father has stent last moth but he’s still have trouble in sleeping and turn left or right and pain in the chest what to do please suggest. Doctor only said walk as much as you can. While walking their is no problem.
Please do reply.
Hi Sanjeev,
I would strongly suggest that you bring these concerns to the attention of your father’s cardiologist. I cannot provide any specific information on my website.
Regarding exercise, if your father is medically stable and has been given clearance to exercise, then he should be able to tolerate low level walking until he’s feeling better.
Kind regards
Dear Doc, I am 35 yrs Male and recently suffered a cardiac arrest and got a stent in the heart. Docs said its a single vessel disease and i suffered this because of my smoking and drinking habits.It happened that i was feeling heavy on my chest so went to the hospital and i suddenly collapsed. They gave me a shock and pumped my heart back to life. Its been a month and i have stopped smoking completely. I use to do lot of pushups everyday earlier and never use to have junk food too. Reports said i dont have cholestral or any other thing. I wanted to know if i can resume back to doing some pushups from now as its been a month. Also as the docs said my other arteries were perfectly fine, what was the reason for me to collapse and is there a possibility of this happenning again. Greatly appecrieate your reply. Thank you!
Hi Chandra,
Thanks for your comment. First, if your cardiac arrest was very recent, you must understand there is still some healing going on inside your heart, both from the heart attack and from the angioplasty/stent placement.
Second, make sure you are cleared to exercise before you start straining yourself too much. Many people feel better after their angioplasties after a week or so, but standard care (depending on the doc and hospital guidelines) is about a month before you can go back to higher levels of exertion. The first few weeks should be low level walking and activities of daily living (doing the shopping, cleaning the house, etc). If you’re at four weeks now, then I would just make sure you get final clearance from your cardiologist to start doing pushups (and any other strenuous activities). It’s not a one size fits all approach and each case is different so it’s for that reason I say to get clearance from your doctor.
Third, you are still quite young and have an opportunity to make lifestyle changes that can significantly reduce your chances of having this happen again. The good news in this case is that it was only single vessel disease. I would assume your interventional cardiologist checked out your other arteries and did not find anything else too remarkable and/or worth stenting. It may be worth your while asking your doc if there are any other lower grade blockages to watch out for in the future. Hopefully not, but always good to keep tabs on these things.
Hope this helps.
Kind regards,
Bill
Hi Dr Sukala,
My name is Mark. I’m a 58 year old male who recently had 4 stents fitted. Diagonal (2x drug eluting stents) and LAD (2x drug eluting stents) arteries following feeling tired and breathless while playing football. I have always exercised, doing cardio and weights etc. The stents were fitted 2 weeks ago via my wrist. I don’t smoke and eat well. I have gone back to the gym, but not going at it too hard Do you think this is wise. Thanks in advance, Mark.
Hi Mark,
Thanks for your comment. The first thing is to make sure you are taking it easy during the recovery UNTIL you have final clearance for full activity from your cardiologist. Since everyone’s medical history is different, I can’t (and won’t) provide any specific information or give recommendations. BUT, I can provide you with some general guidelines and points you can discuss with your cardiologist.
1) Looking at your IP address, you appear to be based in Scotland. The UK has a good system that is progressive, so if you have access to a cardiac rehabilitation program in your area, I would strongly suggest attending. You can gain valuable insights and information that will help you stay healthy for the long-term. Whilst some people view cardiac rehab as being for really sick and frail people, quite the opposite is true. I’d highly recommend it for active, gym-going people because they’re the ones who really WANT to be active and need the guidance on how to do so.
2) The good news in your case, based on what you’ve written, is that you just had the blocked arteries but did not have a heart attack. If this is the case, then you only had a plumbing problem and not a heart problem (i.e., heart attack with heart muscle damage).
3) Generally for the first month after angioplasty/stent, light to moderate intensity walking is recommended for most people (unless there are any medical reasons not to). So perhaps give a call to your doctor or doc’s practice nurse and ask them if they have any guidelines they recommend for their patients. As a rule, most docs and cardiac rehab programs will avoid pushing you to very high intensities during the initial recovery period whilst there is still healing going on on the inside of your arteries. You might feel well after your surgery but you MUST remember that even you feel great, you still have some healing going on. Any sudden spikes in heart rate and blood pressure can possibly disrupt the stents so try not to rock the boat so to speak.
Bottom line: make sure you have a good line of communication with your doc and get guidelines specific to your situation. Being relatively young will work to your advantage and the fact that you were active your entire life.
Hope this helps.
Cheers
Bill
Thank you so much for your prompt and detailed reply ,i will definitely be taking your advice and leave the bench pressing out for a while .To provide people with such precise advice in your own time is commendable .
Thanks again Mark.
Cheers Mark, Happy to help. Feel free to drop back in to the site and leave a comment as you progress through your recovery. Other people can benefit from your experience too. Kind regards, Bill
Hello, Dr. Bill,
Thanks a lot for your amazing effort.
My Mother aged 65. Four months ago she had deep vein thrombosis and underwent angioplasty in one artery and a second was too narrow for intervention but was only 50% blocked. Since then she is following all the usual drugs, beta-blocker, hypertension etc. However, she continue to suffer from high blood pressure, even after her doctor changed the entire course. We tried to carryout nuclear stress test but could not due to extremely high blood pressure, it went to 190/120 for whole four hours we spent at the x-ray center. Her average BP is 180/100.
She is a little bit overweight, with minimum physical activity, and is always stressed due to my father’s death recently.
How to proceed from here?
Thank a lot for your kind reply
Hamdy
Hi Hamdy,
Thank you for taking the time to leave a comment. First off, I’m very sorry to hear about your father. I can appreciate how difficult that must be, plus trying to help your mother get her blood pressure under control. I’ll try to address each of the points you’ve raised in your comment.
1) Regarding the 50% blocked artery, in many cases, doctors will not intervene on arteries with less than 70% blockage. So for now, it is likely something they will monitor over time. Hopefully it does not progress much further.
2) High blood pressure: Blood pressure is one of those difficult things that in some people can be very stubborn even if you do everything right. 190/120 is excessively high and must be controlled as soon as possible. Based on what you’ve written, perhaps you could discuss with her doctors whether a diuretic medication might be appropriate. More information here: https://www.webmd.com/hypertension-high-blood-pressure/guide/diuretic-treatment-high-blood-pressure#1
Also discuss the possibility of getting a consultation with a dietitian who can help her reduce her intake of salt. Some people are very salt-sensitive while others can eat lots of salt and not have any issues with their blood pressure. Getting some good suggestions for healthy eating will not only help her blood pressure but any other potential health concerns as well.
If there is a cardiac rehabilitation program available at the local hospital, then this might also be an important step for helping her gain some monitored exercise as well as information on how to best control her blood pressure.
Though you didn’t mention it in your comment, it might also be worth while getting her blood sugars checked to ensure that she does not have pre-diabetes or type 2 diabetes. Diabetes in conjunction with high blood pressure is a bad combination, so would strongly recommend making sure that any other potential health issues are identified as soon as possible.
I hope this was helpful, but do feel free to come back and leave another comment if you have further questions.
Kind regards
Bill
Hello Dr. Bill,
I ‘m a 60 year old male. Had three stent angioplasty 8 days ago. Three days after my surgery I was feeling well and sexually self pleasured myself. I realized after I was done that my heart rate was quite elevated. This was very stupid I know. The next morning my voice was hoarse and haven’t felt as well since that incident. I’ve had two EKGs since the incident and both my Cardiologist and Primary Dr. are not concerned at all. Becoming very depressed that I’ve compromised the surgery. Do you feel I could have done any damage?
Thanks for your reply
Ray
Hi Ray,
I think the best course of action is to trust your doctors’ judgment. If there’s nothing on the EKG showing anything out of the ordinary, then chances are you’re probably fine. As a general rule, during the recovery phase after an angioplasty, you want to make sure that your heart rate and blood pressure do not climb too high while your heart is healing on the inside. The big question is, was this a case of cause and effect or coincidence. It’s true that your voice was hoarse the day after, but what if it was just a poorly timed virus or bacteria that hit you at that moment? At this point, it’s probably worth giving it another week or so and see how you feel. If it goes away on its own and the EKG is normal, then I wouldn’t give much more thought to it. It’s clearly causing you a bit of stress and anxiety now, but try not to let your mind wander too much. Hang in there and keep in close contact with your medical management team in case you notice anything else out of the ordinary. Hope this helps. Cheers, Bill
Hello, Dr. Bill.
My dad (65 years old, height 160 cm, weight 139 pounds) and is diabetic. Even though he has diabetes, he is fairly healthy and very active, our family has no heart disease history. Turns out he actually had a heart attack 6 months ago, but he didn’t tell us anything at the time because he thought it was just regular fatigue, he just get some rest and pretty fine after that. Finally he told us and decided to check his condition last month and he was diagnosed that he has 70% blocked LCA and 100% RCA! It seemed that the RCA was already beyond fix so the doctor left it unattended and only put 1 stent on LCA. the process was a success, but even after a month my dad doesn’t seem to get better, he tired very easily. I am no doctor, but I am pretty sure it is because his RCA condition. He is on medication prescribed by his doctor, changed to healthier diet and do gentle yoga exercise. I just hope we discovered this sooner, but there is no point regretting the past. Is there anything we can do to improve his condition? Is there really no hope? because we absolutely refuse to think that there is no hope anymore. We just need somebody to talk about this, because too bad, in my country it is very difficult to have consultation with cardiologist, even we have to wait up to a whole month for one.
Thank you for your reply. Nisa.
Hi Nisa,
I can’t really say much about why they left the RCA as is, but they may have had their medical reasons for making that decision. One thing to bear in mind is that, if your dad is able to get out and start with low level walking (if he’s cleared by his doctors to do so), then over time, the exercise can help promote collateral circulation around the blockage. This is where the heart muscle with regular training develops new small blood vessels which may help serve blood to his working heart.
Did the doctors tell you if your father had any heart muscle tissue death? If he had a heart attack, then the area that was blocked and starved of oxygen dies. The rest of the heart can still function, but that region that was starved of oxygen will not survive without oxygen and nutrients. It is possible that the RCA was the culprit for the heart attack and so it may not have been worth putting your father through any unnecessary surgical risk to fix something that is already beyond repair.
The bottom line it that there is ALWAYS hope. I have worked with people who had multiple massive heart attacks and had very low heart function but they were still able to build up to a reasonably high level of exercise tolerance over time. Is it easy? No, it takes some work to get the habit going and stick with it, but if he is able to get up and keep moving, then it will definitely put him in a better spot in the long-term, and will also help manage his diabetes as well.
I would still suggest trying to get a cardiologist consultation but in the meantime try and get your dad exercising even if at a slow pace. Walking is fine. Consider exercise as a form of medicine that will help improve his overall health.
Kind regards
Bill
Your site is very helpful…I see a lot of good information coming from Australia. I am paying more attention since I had a stent put in 11 days ago here in the US. Hopefully just a “plumbing problem” as you so aptly describe.
I am 70 years old and a life long exerciser, most recently walking and calisthenics for back and shoulder issues. Had high LDL for years until statins came along. Most recently tested at 107. Could never do much about HDL, which was typically in the 40’s. Alarmingly, one score in the Hospital during treatment was 26.
My primary physician has said it is difficult to raise HDL (which I knew) but I do have the time and commitment to do what it takes. What do you recommend?
BTW, I will be beginning Cardiac Rehab soon. Thanks, Bill
Hi Bill, Thanks for your comment and sharing your story. There are a few things to consider here. First off, your doc is right. Cholesterol levels can be pretty darn stubborn and the amount of change can vary from person to person. But don’t read this as doom and gloom. Here’s why. Cholesterol levels in general (including all types) are only one single biomarker of many biomarkers and lifestyle factors that affect health. Others are blood pressure, blood glucose levels, inflammatory markers, body weight, waist circumference (how much visceral fat you have), activity levels (how much exercise), diet (how many fruits and veggies you eat), stress levels (how stressful is your lifestyle), alcohol intake, smoking status, etc.
Cholesterol levels are often affected by genetics as well. Some people have low cholesterol levels but can still manage to have heart problems due to other reasons. Other people have high cholesterol but manage to go through life without any heart problems. The point is, a single biomarker is not all deterministic and there are a multitude of factors which contribute to health and the development of disease.
Working in cardiac rehab, I have seen lots of people who had only a single risk factor but still managed to have a heart attack, and I’ve seen other people with lots of risk factors who did not have a heart attack. Sometimes bad stuff happens to good people and another times bad people dodge a grenade.
As for why you ended up with a plumbing problem, it’s tough to say. Yes, it’s true your cholesterol levels are a bit stubborn, but there could have been other factors working along with it. The other thing to consider is that you are a life-long exerciser. Perhaps you’d have had a heart attack in your 50s had you NOT been an exerciser. See what I mean? And looking at the bright side, at least you only had the plumbing problem and not the heart attack (with damage to your heart muscle).
Bottom line: yes, do cardiac rehab and leverage on the knowledge of the staff there. Ask questions. Lots of questions. They will be most familiar with your medical history and can give you the best available information relevant to you. As for your HDL, I wouldn’t recommend getting fixated on just that single number. Try to control as many risk factors as you can (mentioned above). By default, many of those healthy lifestyle habits will give you the best available shot at bumping up your HDL, and even if it doesn’t move much, it will affect many of the peripheral factors which might work in conjunction with HDL to help improve your health and reduce your risk of any future events. Hope this helps.
Best wishes
PS, I removed your last name from the post to protect your privacy
Dr Bill,
Thank you for your quick and thoughtful response. I am going to try to drop weight which I mostly carry around my middle and up my walking now that the weather is getting nice here in Washington DC. I sloppily added about 15 lbs in the last few years to 198 on my 5’11” frame.
I am now on an 80 mg dose of atorvastin, so my primary care physician thinks that even if my HDL doesn’t go up, the lower LDL will give me a more favorable ratio. Do you think that will help?
I am doing the Mediterranean diet and have eliminated processed sugar. Other steps I might consider?
Incidentally, your comment about a heart attack that might have been avoided in my 50’s rang true. My grandfather died of a fatal attack at age 52.
Thanks, Bill
Hi Bill,
It sounds like you’re on the right track then. As a general rule, weight loss, in particular weight loss from the mid section, is associated with overall improved health outcomes over the long term. If you lose the weight and keep it off, then you’re well on your way to keeping the doc away.
As for your cholesterol ratio, I agree with your PCP. HDL is protective, but even if it doesn’t budge much, then getting down your LDL and improving your ratios will work to your advantage most definitely. But remember as I said in my previous response, health is not only about cholesterol levels. It’s just one piece of the puzzle. Best to be aware of it, but not obsessed with it.
Mediterranean diet is an EXCELLENT choice. Honestly, in my professional opinion, I find it to be one of the best because it emphasises everything that is good for health. Lots of fruits, veggies, whole grains, monounsaturated oils etc. Now, with the awareness of the gut microbiome (your gut bacteria) and its role in health being better understood, we know that a diet such as the Mediterranean diet which is high in fibre helps promote a favourable balance of good bacteria in your gut and helps control the bad bacteria. Think of your gut as a diverse rain forest. You want as much diversity as possible. So yes, Mediterranean diet is an excellent choice and will serve you well. Just remember all things in moderation and you’ll be fine.
Sorry to hear about your grandfather, but yes, if I was a gambling man, I’d bet that you probably delayed any heart issues that might have hit you earlier due to your physical activity levels. Exercise promotes the development of little blood vessels around the heart called collateral circulation. Collateral circulation can really help improve overall blood flow to your heart muscle so, in some people, even with rather serious blockages in the main arteries, their collateral circulation can really help reduce the impact of those blockages. Here is some light reading for you on the topic: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689049/
Hope this helps. Feel free to stop back and leave more comments about your experience with cardiac rehab. A lot of people really appreciate the comments section of my cardiac articles because of all the first hand experiences. Have a great day! Cheers, Bill
Hi Dr Bill,
I am regular reader of your blogs and try to implement as much as possible . My angioplasty failed last June17 and since then I am on heart medication as I have good collaterals.Cardiologist recommended CABG but looking progress last 8 months he is now satisfied with optimal medical therapy . Earlier my stress test excercise time was 7min and now my excercise time has gone up to 9.15minutes . In addition to standard heart medications which match with your article, I am on vegetarian diet as per Dr Ornish’s life style recommendation . I walk daily 60 minutes . My walking speed varies from 5.5kmph to 6.2 kmph . I did not face any difficulty . Checking HR from portable BP monitoring equipment is difficult but do you suggest 5.5 kmph to 6.2kmph is good speed to encourage more collaterals so that I can pass the next stress test
Hi Arnab, thanks for your comment. There is no set in stone rule about what constitutes an ideal speed for developing collaterals. If your speed is hovering between 5.5 to 6.2 kmh and that is comfortable for you, and you’re able to maintain it for an extended period of time, then it will most certainly help you build more collateral circulation. Remember, it’s not about having to go out and crush yourself. If that range of walking speed gets your heart rate up and you feel like you’re at about, say, 70 to 80% of your maximum effort, then it’s just a case of sticking with it over the long-term. I’ve seen patients with good collateral circulation not need to have further intervention because of their fitness levels. Best bet might be to speak with an exercise physiologist in your area and get specific instructions relative to your condition. Hope this helps. Kind regards, Bill
Thanks Dr bill for your prompt response . I am surely going to look for an EP in my area as cardiologist’s comfort is on surgical side whereas collateral is the hidden treasure within our body itself . we undermine this treasure and look for short term relief . I measured heart rate today it came as 120 .My age is 49 so it is around 71% . I have connected you in few collateral related research discussions in your twitter account . If you find it interesting I would love to see few tweets . Thanks a lot once again
Cheers Arnab, most appreciated. I am not on Twitter very often these days, but will have a look at some point. Best wishes
I m 46 and a hard sportsman, faced heart problem due to CAD. Echo reveals heart is safe. Two drug eluting stents are placed in LAD and RCA. Procedure is done 5month ago. Now I am on dual anti platelet therapy(plavix +Aspirin)2.5 beta blocker and 10mg statin. My questions are :
1- For how much time I have to continue with dual anti platelet therapy?
2- How much time I have to continue with statin if lipid profile is ok.
3- i have continued to play badminton, To what intensity i can go hard or medium?
Hi Amer, Thanks for your comment. I can’t answer your first two questions legally or ethically since 1) I am a clinical exercise physiologist; and 2) I am not full familiar with your entire medical history. I would suggest you speak to your cardiologist to determine what are appropriate time frames for you.
On your third question regarding playing badminton, I would recommend two things: First, find out from your cardiologist how risky he/she feels it is for your to be performing higher intensity exercise. I would suggest asking for a maximal treadmill stress test to see how your heart performs under high intensity exercise stress. Second, if you are able to find a clinical exercise physiologist in your area, he/she would be able to work with you more closely to determine the best training and competition intensities to best suit you.
I apologise that I’m not legally able to give medical advice here, but honestly, your best bet is to try and work closely with your cardiologist and an exercise physiologist. That will get you back and playing sport again, without the worry. Kind regards
This is brilliant – the most comprehensive, clearly (and well) written exploration and explanation of post-angio exercise and care I’ve encountered. Congrats in it!
Thanks John, glad you found it helpful.
Dr Bill,
I last wrote in on April 6th, soon after I had a stent put in. I was just beginning a regimen of 80 milligrams of Lipitor, Plavix and Topril. My cholesterol has dropped with LDL going from 107 to 47! However, my HDL is only up a bit from 26 to 32.
My cardiologist is pleased with these results so I am too. I have also dropped 10 pounds and hope to lose 5 to 7 more. Upped my walking a bit – hopefully this new religion will last.
My issue is that I would like to take Alleve or another NSAID for all the arthritis I have inherited from playing sports badly over the years. Before the stent I would take Alleve for a day or two at most which made me feel several decades younger. However, more than a couple of days led to a rapid heart beat. Would it be possible to take it occasionally now? Is there an alternative?
Thanks, Bill K
Hi Bill,
Thanks for stopping back and leaving another comment. If you’ve lost 10 lbs then it makes perfect sense that your blood lipids are improving. In general, weight loss tends to have a positive effect on most blood biomarkers. Losing more weight may give those numbers a little more of a nudge.
Regarding Alleve, I legally can’t tell you what to do one way or the other, but I would suggest speaking to your doc and exploring which options might best suit you. Also consider other types of exercise which do not have a jarring effect on your body (swimming, cycling, elliptical trainer’s etc). And remember that losing weight will also help reduce stress on your joints and may confer some relief too.
Keep up the great work.
Cheers
Bill
Hi Bill, your blog is really helpful and informative. I am 50 and got my first stent with Magmaris to fix my 70% stenosis in LAD 6 months ago. However, I got chest pain 4 months after stenting. I have just got another DES at the same site and OCT analysis shows it is 90% closing up/collapse of the Magmaris stent. Three weeks after second stenting, I still feel numbness in my right hand and right leg and sometimes abnormal heartbeat (something like premature beat). Is it common during the early healing stage or a symptom of injured heart muscle or valves?
Hi Kevin,
Thanks for your comment. First thing I’ll say is to make sure your doc knows about the symptoms you’re experiencing. The best defence is knowledge and your doc and medical management team are going to be best qualified to help you with these sorts of things.
Second thing is that I have seen a number of people with quirky things like this (numbness, arrhythmias etc), which can happen when they’re poking and prodding with catheters into delicate coronary arteries. So rest assured, it’s not uncharted territory. But as I mentioned above, it’s very important to be in close contact with the doc and the rest of the medical management team (practice nurse etc) in order to make sure that there’s nothing more sinister brewing (not that there is, but you just want to get the best information). Also remember that you’re still reasonably early in the recovery period and in many cases, these things will resolve with time. Feel free to stop back and leave another comment as you go through the healing process. Many people reading through these comments can benefit by learning from others’ experiences. Kind regards, Bill
Hi dr bill. I am 50 y .can i take umega red after stent.
Hi Lalit, I’m not exactly sure what umega red is, but I assume it’s Omega Red which might be krill oil or something. I would strongly recommend you speak to your doctor about this because fish oil capsules can interact with certain medications often prescribed after angioplasty/stent. Each person is different so I cannot give any specific guidelines here, but it’s best to speak to your doctor because he/she will be most familiar with your specific medical history and can let you know if it’s appropriate to take Omega Red. Kind regards, Bill
Dr. Bill,
I wrote to you in early April after I had a stent put in. Fortunately it was a plumbing problem and not more.
Soon after I started a very good cardio rehab program in the Washington DC area. I was a bit of a star pupil if only because I was not 60 pounds overweight like some of my classmates. I am now 184 on a 5′ 11″ frame, down almost fifteen.
Upon my graduation a month ago, I was encouraged to keep increasing my walking exercise to an hour a day as well as to continue calisthenics (up from thirty to forty minutes). Also to push my heart rate up to 150 bpm.
I had a very positive meeting with my cardiologist who agreed with this approach and said I should continue to drop weight until I reach 178 as suggested by the body mass index.
As I strive to do so, I sometimes complete a workout and feel slightly light headed and also a bit warm across my shoulders. Is this a form of mild angina? I am obviously more sensitive to anything that might be a symptom or merely fatigue. If it is angina, it would seem to be something that I might cope with given my recent clean bill of health. Is this something that a lot of people deal with?
Further, I am on a lot of meds: Toprol – 50 mg, Atorvastatin – 80 mg, Plavix – 75mg and aspirin – 81 mg.
I have been forgetting more stuff even as a 70 rear old than I did before the stent (like losing my phone 3 days in a row). Is this common?
Finally, the amount of toprol I am on makes it difficult to push my heart rate up to 130 and the goal of reaching 150 seems a real stretch. My knees and back will give out first:). Is this typical?
Thanks, Bill
Hi Bill, thanks for stopping back to share your story and ask some questions. First thing to remember, as you pointed out, is that beta blockers (Toprol) can really kick the stuffing out of you and make you feel sluggish. While I always say I have no undying love for the pharmaceutical industry, there are instances where they are appropriately prescribed, and after an angioplasty/stent is one of them. However, it may be worth having a talk with your doc about formulating a plan together to help slowly bring your dosages down a bit lower (as appropriate to your particular medical history). I’ve heard what you’re saying from a lot of people on beta-blockers and, if you’re having a hard time getting your heart rate up, then rest assured this is normal. In this case, you may want to work on the Rating of Perceived Exertion scale (or effort level) instead. This is going to be more meaningful if you’re on Toprol. As for your feeling of light-headedness, this could be due to you pushing yourself during exercise – something that could happen to anyone. If you’ve been given a clean bill of health from your doc and these are just exercise-related discomforts, then they’re likely nothing to worry about (but make sure you get that confirmation from your doc and no one else). Hope this helps. Feel free to stop back any time to leave another comment. It’s helpful to see other stories and perhaps glean some insights. Cheers, Bill
Hi Bill had a stent put in 2 weeks ago and I can’t get on a rhab for 4 to 5 weeks. I am a man 56 years old with with a good fitness level before I have my stent.
Hi Keith, I think your message might have been cut off. Did you have more to add? Cheers
I find all this information helpful but leaves me with more questions.
I had a stent in my LAD on July 19th this year. The cardiologist said he will also be watching another artery that is partially blocked but not enough to put a stent in it.
He said I could go back to my regular training. I am a triathlete and 72 years old. How do I know if that is safe? I’ve been training slowly raising my HR when doing intervals. I have no chest pain.
The doctor didn’t give me any guidelines.
Hi Shirley, Thanks for your comment and questions. In my experience, cardiologists tend not to intervene if there is less than a 70% a blockage in the artery. Assuming the blockage is stable and it is not causing you symptoms (i.e., chest pain, shortness of breath, etc) and your cardiologist has cleared you for exercise, then what you’re doing with gradually increasing your HR is probably appropriate. It may be helpful for you to have another talk with your doctor or medical management team (i.e., the practice nurse at his office) and learn a bit more about what the percentage blockage is. If it’s around, say, 30% then you will probably be ok. Also consider that due to being a triathlete, you may also have what’s called collateral circulation around the blockage which are like alternate blood vessels that deliver blood to the area served by the blocked artery. Bottom line: knowledge is power and it would be helpful to have another talk with your doc or perhaps even get a referral to a cardiac rehab for a few sessions where they can monitor you on telemetry under higher workloads. Feel free to stop back and leave another comment to let us know how you went. Kind regards, Bill
Had two stents fitted. the miricle cure.
It’s hell on earth, just a slow death sentence. I used to cycle everywhere, go hill walking and now I can’t walk for more then 15 mins without needing a rest, let alone get on my bike.
Oh give it time they say, as they bump me full of drugs. Months and months later I sleep 16 hours a day. it’s a horrible slow death
The beta blockers can really be tough. Perhaps talk with your doc about eventually working down to lower doses.
Dr Bill
Firstly what an uplifting site this is I am so pleased to have something so positive in its tone and full of gentle encouragement.
I have had a rather rushed experience in the diagnosis of CHD, one week ago had a stent in LAD with investigation (but no procedure) of another area. I seriously need to lose weight and improve exercise, family genetics are also in the mix. I am currently off work and will make every effort to take up rehab and build up stamina.
I just wanted to say thank you for the time you give to answering questions so clearly. I have read through the site avidly in one setting.
I so want to recover some optimism and belief in the future I didn’t have a heart attack and am on the usual cocktail of drugs plus some due to thyroid problems and previous history of DVT/pulmonary embolism.
No question as such but any comments welcome
Many thanks for the very informative post!
What are your views on the use of Vitamin K2 and D3 supplements after an angioplasty? There have been a number of research studies that have shown evidence of arterial blockage reversal. Any insight would be most welcome.
Hi Shahid, I have seen this come across my radar in the past but have not dug deep into the specifics. I did a quick search and came across this article, which was done in pigs and showed favourable results: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4894559/. In general, I still think the best person to speak to would be your cardiologist to ensure there are no risks specific to your medical history. Cheers.
Hello Dr. bill. My father had a stent restenosis in his LAD, its now almost 3 months that his BP remains at 140/80.he had no history of High BP before, his lipid profile is normal, takes anti statin drug, beta blockers, omega 3, but still his bp is high despite of taking anti hypertensive drugs. He had a BP of 110/80 before the angioplasty. Is it normal or something is wrong . Thanks
Hi Iqbal, Thanks for your comment. Sorry to hear your father is having a rough time with his blood pressure. It’s hard to say exactly what’s going on so the best advice is to speak with his cardiologist and perhaps have a follow up evaluation. Obviously we’d like to see his BP back down to 110/80, but even at 140/80, it’s not astronomically high (still higher than we’d like but not like 220/110 or something). However, the only person who should be providing advice to your dad is his cardiologist who will be most familiar with his medical history. Kind regards, Bill
Hi Bill,
Hope you are doing well. This is Nasir from Pakistan. Sir I am 32 years old. A few months back I started getting chest pain and I was not aware that it was angina. I visited a nearby heart hospital and found out that my LAD was 50% blocked. It was diagnosed via CT angio test. Dr recommended to have angiography as its main artery went for it and came to know that LAD is 90% blocked so had to put in a stent.
After the procedure, I am having back pain some time chest pain and most importantly burning right above the heart. Visited my Dr for couple of times and he did different tests like ETT and ECHo and mentioned that everything seems ok and its somewhat cardio phobia and recommended me to just relax everything is ok. Lastly he said that if you want 100 percent clarity in that case again ct angio needs to be done which he dont recommend as stent was placed about 2 months ago.
Hi Nasir,
Thank you for your comment. Sorry to hear you’re having some chest pain after your procedure. I have worked with a number of patients who have also had some discomfort after an angioplasty/stent, but this subsided over time. There may be some post-operative anxiety which is reasonably normal considering you were having chest pain (scary stuff!). Your doctor is going to be most familiar with your health and can give you the best advice. When you have chest pain, can you change positions and get the chest pain to go away? Or if you sit down and relax while you’re having the discomfort, does it tend to go away then? Usually if the chest pain resolves due to changes in position, then it “may” be related to tension. I would suggest that if this keeps up, then you may need to ask your doctor again to have another angiogram to be sure, but try to view that as a last option and see if this discomfort is temporary and will go away on its own. Bottom line: keep in contact with your doctor and write down each time you have discomfort and how long it lasts for. If it becomes more frequent, then you might be able to get another angiogram. Hope this helps. Kind regards, Bill
Hi Doc, Before MI I already lost 80 lbs. Always at sport(before HIIT training).Now i’m 43 yrs/165lb/5.7″. 40 days ago I got a STEMI in distal RCA (RPL) and 7 days after that a nSTEMI (99% blocakage in RPL PVB and RPL #2). So total 5 stents. on Stemi day, EF is 60-65. after N-Stemi EF is 50. There’s mild hypokinesis RWNA.
Two weeks later I’ve Nuclear stress test done and passed with METS 11. The damage is at the bottom of the heart. LV stress extent is 15% in RCA/LCX. LAD is clear. I’m in Cardiac rehab now (love it) and I check my Vo2max can reach to 44-47. Most days I walked 4 miles (more than 2-3 days prior to MI). What do you think ?? My most HR during exercise is 120-140bpm. Resting HR is 50. Blood pressur 90% is always below 120/100 (mostly in 100s). I’m on Brilinta/aspirin only. Doc afraid to give beta blocker becoz my BP and RHR is normal.
Hi Carlos,
To be honest, you’ve done everything the right way. I often tell physically active people that the best place to go is to cardiac rehab so they can keep an eye on you at different workloads and ensure that everything is within normal limits (particularly if they use telemetry monitoring while you’re exercising). Keep up the good work. Cheers
Hi, Doctor Sukala,
I came across this website by accident and was amazed at your generosity to take time in answering a lot of questions. I learned a lot from your answers.
I had a STEMI while lifting some weights. My LAD was 100 % blocked and my troponin level was 80 and counting upwards.. That was 4 years ago in Dec.2014. I had a stent (DES) and was put on Clopidogrel,aspirin, beta blockers antihypertensive and antihyperglycemic meds. My doctor told me that 50% of the apex of the heart was damaged and NOW my LVEF is around 45%. I am also obese at 210 lbs.
But the good news is: I am asymptomatic. I have no issues but I do want to reduce my weight and have been walking 30 minutes a day. My weight will not budge and I am also scared of doing more.
Can you please give me some advice. Anything will be appreciated.
Thank you for your comment. The good news is that your surgery was some time ago. If your doctor gave your clearance to exercise, then this is the first step. You do have some compromise to your left ventricular function, but not enough to necessarily put you in congestive heart failure. In fact, if you have some LV compromise, then it would be in your best interest to reduce body weight (to take strain off the heart). The big question is doing so safely. I would suggest keeping with your walking as you’re doing, provided you are asymptomatic, and perhaps make an appointment with a clinical dietitian from the hospital. Looking at your IP address, you appear to be based around Ontario, Canada, so there should be a number of options there for you (as opposed to some of the more regional areas). Be sure to stick with a university-qualified clinical dietitian who has training in helping people with medical issues (there are lots of quacks out there pushing all kinds of rubbish). You’ll want to increase your intake of veggies and fruits which will provide nutrient density (lots of fibre, phytonutrients, vitamins, minerals), but without all the excess empty calories (i.e., Coca-Cola, chocolates etc). You might also consider getting a referral to a clinical exercise physiologist with experience in working with people with cardiac issues. This way you can get proper guidance on exercise intensities. Once you have your eating and exercise sorted out, if you’re having any anxiety about your health, you might also benefit from a social worker or a psychologist who is trained in helping people with medical concerns. Remember that this is a slow process so do not think you’re going to lose lots of weight in one day. There are lots of quacky quick fixes out there that will tell you whatever you want to hear, but in the end, they’re only ripping you off and leaving you worse off. Feel free to stop back if you have any questions. Kind regards, Bill
Thank you for response. I have already taken the first steps.
God bless
Sir.,
Very useful information.
I like to get reply for my following doubts.
I am 52 years old Male.
I had one stent just before 6 weeks .
A. Is it possible to get back our original (ie. Condition before angioplasty) heart health by any means..
B. If any one of our activities leads to over load to our heart , will it give recurring impact …
Hi Jawahar
Everyone is different, so your best course of action is to discuss your condition with your doctor. I have seen people with angioplasty go back to living their lives as normal, except with making better lifestyle decisions (i.e., not smoking, eating more fruits and vegetables, etc). You might also consider asking your doctor for a treadmill stress test to determine what kinds of intensities your heart can handle. If you have no signs or symptoms, then you may get clearance to exercise at higher workloads. Bottom line: speak to your doctor as he/she will be most familiar with your entire medical history and can give the most informed answer. Kind regards.
Hi doctor..
This is Sonia i am 65 yrs old …my weight is 74.5 kg i lost 8 kg from 2016 to 2018
I had an Angioplasty and 3 stents as i had a heart attack…that was August 2016…and i am taking blood thinner berlinta 90 and asprin 81 Rosuvastatin 20mg bisoprolol 5mg and candesartan 16mg
I am not walking regularly …..i walk 4 to 5 times a week..my pulse is between 55 and 65….
My blood pressure now the average is between 120/60 and sometimes over 70…
I feel i have no energy…and sometimes i feel short of breath…is this normal …please advice me..
thank you
Hi Sônia
I would encourage you to speak to your doctor as s/he will be most familiar with your entire medical history. Sometimes beta-blocker medications can make you feel sluggish so perhaps discuss your current dosages with your doc to see if they might be able to make some adjustments. Kind regards
Sir I have a stent in my descending aorta.Can I have kickboxing training?
I can’t really answer that. The best and only person whose opinion you should rely on is your doctor who will be most familiar with your particular medical history. If you’re taking blood thinning medications, then that could have an impact on your doctor’s willingness to let you do contact sports. Kind regards, Bill
Hello sir
My name irfan. I had an angioplasty 6 months ago and put in 2 stents. Sometimes i feel discomfort but not more. Before angioplasty my weight was 108 kg and now my weight is 76 kg. I walk every day almost 15 to 18 km. As these weight enough or not??
Hi Irfan, It sounds like you’re right on track. Keep up the good work!
Hello sir
My name Ravi I had 3 stents one year ago. When I had stents at that time, I couldn’t walk for 3 months because I felt pain in my chest and my body then I went several times to my doctor and he told me every thing ok and not to worry. I don’t think to much after 3 months I was start walk normally. Now I walk more 7 km every day after 1 year but now I have pain in my left hand and my stomach feel bloated left side. But I can walk more than 7 km now mind says when I pain I fell I have some blockage inside I can’t take my head now please advise me sir
Hi Ravu,
I would strongly recommend you get a second opinion just to be sure. If you’re having left-sided pain when you’re exercising then this is worth getting checked out and having a cardiologist run further tests on your. Minimally, a cardiac stress test on a treadmill. If that turns up any abnormalities on the electrocardiogram, then you might be sent for a catheterisation to visualise the coronary arteries of your heart to determine if there are any blockages (and the extent of those blockages). Obviously I can’t give any medical advice over the internet, but based on your comment, it would be smart to have further workup with a cardiologist just to make sure that there is nothing more sinister happening inside your coronary arteries. Hope this helps. Kind regards, Bill
Thank you sir for the advice. I went to the doctor and he told me you have to do cardiac exercise treadmill test. I did the treadmill and everything was normal.
Hi Ravi,
This is good news. It is always best to get a proper medical opinion on these sorts of things. At least you will be able to sleep well at night knowing it is not your heart. Kind regards
I had a chest pain in 2006 but I delayed taking nitroglycerin by 12 hours. My angiography was botched up in a Turkey hospital.
Later I had a triple bypass surgery. I continued active life as a marine engineer on ship till 2016.
In Jan 2019 I got chest pain. Eventually I got one stent put in. I feel shortness of breath.
I am diabetic but take medicines as follows:
Atorva 40 mg x once
Brilinta 90 mg x twice
Ecosprin 75 mg x once
Vymada 50 mg x twice
Per day
Still after putting one stent in, one of my arteries is 100% blocked which could not be cleared. I am 5 feet 9 inches tall and weight is 155 pounds. Apart from shortness of breath I have no pain but I get stressed easily. Kindly advise. I am on low fat diet no alcohol since patenting and non smoker. I walk for one hour. Climbing steps cause shortness of breath but not severely. At night mouth is dry and urinate twice at night. Kindly advise for shortness of breath. Thanks. I live in New Delhi India. I am almost 70 years old. I worked at sea for almost 45 years.
Hi Vijay,
Thanks for your comment. It sounds like you have a number of things going on. Whilst I cannot give specific medical advice online, I can tell you some things you may wish to discuss with your doctor to help guide your recovery.
First, you had a stent placed in January of 2019, so you’re not too far removed from the recovery period. You mention you had chest pain but it would be good for you to ask your doctor if you had any damage to your heart muscle (i.e., were your troponin levels elevated? Was there any change to your ejection fraction?).
Second, your Vymada medication is for your blood pressure. Blood pressure medications in general can make you feel a bit tired, and the fact that you’re recovering from everything else, this might account for why you’re tired.
Your dry mouth and urination at night might be related to your diabetes, so you should ensure that your diabetes is well managed. The better managed your diabetes is, the less likely you are of having any further cardiac problems.
You should speak with your doctor about these symptoms and perhaps discuss the dosages and what can be done to alleviate your symptoms. But as I said, remember that you need to give it time and let your body adjust to all this. You might find in the next few months that you’re feeling much better.
Hope this helps.
Kind regards,
Bill
Good Day Doctor Sukala,
thanks for your quick reply. My ejection fraction was about 45 % from the time of my bypass surgery in August 2006. After stenting on 14-01-2019, my EF remained at 45%. I have a nasal congestion problem also. Can this cause breathlessness.? When I sleep on my left side, I can feel my heart beat like palpitations. I am also taking thyroid medicine 25 mg every morning. Feel more breathlessness when resting sometimes. My heart muscle was observed to be damaged in 2006. Kindly advise. I am planning to consult my cardiologist this week.
Hi Vijay
Your nasal congestion could possibly make breathing a little more difficult for you. Again, the best thing would be for you to discuss all of these things with your doctor. Kind regards
Excellent.
Doctor you are generous.
May God bless you.
Hi Dr Sukala, I have my angioplasty 3 days ago and didn’t really get an a satisfactory answer to the question about when and how to start exercise. So I just wanted to say thank you for this article.
Hi there, and thanks for your comment. Before you go plowing into exercise, I would suggest speaking to your doctor or cardiac rehab team (if applicable) about getting clearance for exercise. Once you have clearance, then it’s important to ease into it as I outlined in my article. Hope this helps. Kind regards, Bill
I weighed 400 plus pounds at 45 and was basically a weightlifting beast. Was told to do cardio and had a heart attack in the gym. Had a quadruple bypass. I went back to the gym starting with a stick, took better care of myself, no smoking, eating right. My body weight slowly went down to 315 and my weights slowly climbed. Until I was squatting 400 or more for 10 reps, shrugs of 600 pounds (freeweights) reps of 10. My doc never realized that if I added just a couple of pounds a week, in a few years, I would be back. Regular PET scans, a cath 5 years ago, all have been fine. Almost 15 years to the day of my heart attack, 2 weeks ago, my PET scan showed abnormalities. They cathed me yesterday and did a 2 stent intervention with arteries on the BACK of my heart. I feel awesome. Here is the thing Doc, right before my PET scan, I was dong heavy weights. 550 pound shrugs, 320 pound pulls, 100 plus dumbbells for many reps on bench. The only thing was, I would be tired after lifting and nap! So I am 60 and not willing to give up. I started lifting when I was 10… that is 50 years. It is my mental health.
Can I get back in the saddle and not worry about crushing the stent in a few months? I did not have a heart attack, just not the greatest plumbing. Even my first attack cause very very little damage. I kinda feel like if I was going to rip plaque, it would have been on the 560 pound ten rep shrug a month ago. I laughed and threw that freaking weight. I would like an opinion fully aware you are not my physician and it’s like buds talking. I will follow my cardiologist of 15 years, but if I can have any ammo to keep living the life i love, it would be helpful ? My son just took the MCATS!
Hi Jay,
Wow, sounds like a lot of things happening. First thing I’ll say is, active people are usually the worst at following doctor’s orders (including myself!). If you’re physically active and it’s a big part of your life, then having a heart problem and surgery can really put a cramp in your style. If you’re physically INACTIVE, then it’s really no change to have to sit still for a while.
The first thing to remember is that they JUST did a stent the other day, so whether you like it or not, you’re still in recovery mode. Listen to the doc for now and don’t go being a hero. Nearly every time I saw someone have problems after an angioplasty/stent was when they went against medical advice and tried to be a hero, overdoing it, and then ending up back in the hospital. So now that that’s out of the way…
Once you’ve healed up, the chances of your stents collapsing is quite small. Theoretically possible, but it’s not that common. I would suggest talking to your doc about having a proper stress test after you’ve had a month or two of healing. If you can tolerate quite high workloads and there are no untoward signs or symptoms on the ECG, or shortness of breath, chest tightness, etc then your doc might give you the green light to get back to weight lifting. You might also request a referral to a cardiac rehab so they can work closely with you to help keep you on track and guide your progress safely. If they have continuous telemetry monitoring, then that’s even better. They can check your heart rate and blood pressure at different workloads and see if you’re within normal limits. The other thing is which meds you’re on. They can also keep your blood pressure and heart rate down a bit, but the trade off is you may feel a bit more tired and sluggish.
Bottom line: have a good talk with your doc and try to work together as a team to get back to where you want to be. If you can work with a cardiac rehab team, then that will give you lots of good ammo to have a talk with your doc. And if after a month or two you can get a max treadmill stress test then you might get the green light to start back lifting heavy again.
Hope this helps.
Cheers
Bill
Hi Dr. Sukala – neither my cardiologist or the articles online seem to be able to answer this question: is there any danger to sustaining a maximum heart rate with 3 stents implanted. A little background: I had a heart attack at age 61 while running. Had to be revived twice by paramedics. At the hospital they inserted 2 stents in one artery, and one in another. Just 60 days prior to that, I passed a treadmill stress test with flying colors. I had been on and off statins for years because of a family history of heart disease (my father died of a heart attack at age 58). Prior to my heart attack, I had maintained very good physical conditioning (albeit with body fat 23-26% which I am now working to reduce to 15-20%), having run 3 marathons and always on a regimen of running and lifting. Never any outward signs of heart problems, except little did I know that I had blockages of 90%, 90% and 70%. I’ve had one nuclear test since insertion and I look very good. They took me off beta blockers, but I continue with Atorvastatin (40 mg) and low dose aspirin (81 mg) daily. My diet has always been minimal red meat, but never really concerned about much else. Today, no meat, lots of seafood, vegetables, minimal sugar and fats. No side effects except it took me a long time to rehab (through weight training) my left arm/shoulder strength and a neck disk issue due to going down hard when the attack occurred. Since the attack in July 2017, I’ve run two competitive races (this first was tough but it was 7 months after the incident), and in the 2nd, I won my 10k age group. My cardiologist would rather I take things a little easier and says that my pre-attack conditioning may have helped mask tell-tale symptoms, and that my current conditioning may be allowing me to do things sedentary or low-exercise patients cannot do. He says there aren’t a lot of similar cases in the journals. I am scheduled for another nuclear test next month. Sorry about the long story, but my main question is whether heart attack + stent patients should be concerned about maintaining a heart rate of 85-90+% of max for 30, 60, 90 minutes? I use the Kavonen or livestrong.com max heart rate (MHR) calculation method for athletes. Thank you in advance. I like you detailed and thoughtful answers.
Hi Bill,
Thanks for your detailed comment. It certainly sounds like you’ve been through the wars with everything that’s happened. A few things caught my attention, with the first being that you passed your stress test despite having a cardiac event shortly after. I wouldn’t say this is common, but I have seen it more frequently in those who are quite fit and have what is called collateral circulation. Based on what you wrote, your cardiologist probably explained this to you, but for others reading this, collateral circulation is when you have blockages in the main arteries but due to regular exercise, additional “collateral” blood vessels form around the blockage as an alternative circulatory pathway. It’s the reason why you can have reasonably large blockages yet have no symptoms like chest pain or shortness of breath.
In answer to your question, while it’s tough to say whether or not you’ll be able to get back to sustaining your max heart rate, the patients I’ve seen in the hospital that were able to tolerate quite high workloads were those people who had a long history of serious exercise. I once had a guy who had three serious heart attacks at different times and had quite advanced congestive heart failure. But because he was so fit from all of his cycling, he was still out and doing long rides, some part so which were quite high intensity. The rest of his body was so fit that it compensated for a compromised heart.
Moving forward, once your doctor deems you clear to exercise, I would strongly suggest working with a cardiac rehab team that offers continuous telemetry monitoring. They can help guide you onto the higher intensities and keep a close eye on your ticker for any rate or rhythm abnormalities. The other thing I’d suggest is working closely with your doc regarding the results of your nuclear test and, if the arteries are stable and clear, then your doc might give you the green light to perform sustained high intensity exercise again.
I think the other factor to consider is that exercise in itself carries an inherent risk – whether you’ve had a heart attack or not. And when you weigh out the risks versus benefits, exercise more often than not wins out. Bottom line is to work closely with your doc and if all the nuclear scans come back clear, then I’d say to work closely with a cardiac rehab in your area and gradually work back up to the higher intensities.
One final thought. Regarding calculations, remember that calculations will offer you a best guestimate of what your theoretical max heart rate is. However, you will want to rely on a max treadmill test to get your actual MEASURED max heart rate. Then work on your percentages from that. Most people tend to fall in line with the prediction equations, but there are plenty of people (myself included) for which the prediction equations do not really apply. Some people can exceed their predicted max HR and others do not reach it at all. So if you’re able to get an actual measured max heart rate then even better.
Hope this gives you some things to discuss with your doc.
Kind regards,
Bill
I’ve changed your last name to an initial to protect your privacy.
Hi Dr. Sukala
I’m a 47 year old male and I had a two stents one month ago.
Doctors told me one was 100% blocked and other 75 percent!
Now I’m taking these medications:
Pulcet, Plavix, Aspirin, Nebilet, Telmotens and Ultrox
My BMI is 24.2
I have quit smoking.
I’m trying to change my eating habits and I want to start getting more exercise as well, but I’m tired so much of the time and I also I feel some small pain in the back or in my chest and some times when I lay down I feel my heartbeat.
My Heart Rate is low between 50-60 bpm.
You think these conditions are normal or or require more attention.
I’d appreciate any advice you might have!
Thanks,
Hi Vangjush
Thanks for your comment. You’re currently on meds which will affect your blood pressure and these can make you feel quite tired. Perhaps it’s worth speaking with your cardiologist about the dosages and let him/her know you’re experiencing these side effects.
Remember that it is still early days after your angioplasty so it’s not uncommon to feel tired at this point. Try to get out and be active, as this will help you feel a bit better.
In general, I would strongly recommend working closely with your cardiologist through the recovery period and discuss the feelings you’re having. Perhaps there may be some room to adjust your meds a bit so that you’re not feeling so sluggish. In general, people start to feel better after a couple months now that your blockages have been treated and your heart is getting lots of blood flow.
Hope this helps.
Kind regards,
Bill
Hello Dr Bill,
I recently had a heart attack (12 days ago) and subsequently two stents put into my LCA. (I had a blockage of 90%.) Like some of the others I experienced little to no issues while exercising unless I went to extreme levels. So I just backed down thinking I was pushing too hard for my age (59) I was at the hospital in minutes and was told I have minimal damage that will heal. So by God’s grace they went to work quickly and saved me.
My lipid panel came back normal/optimal, my weight and fitness level is at the best ever (I wear clothes that I did when I was 18) and I eat well. My resting pulse was in the mid 60s-70. So … thinking I have elevated levels of lp(a) or something genetic going on.
I am on lipitor, a heart med to control heart rate/BP, aspirin and Brilinta. I started walking, am entering cardiac rehab soon. I am experiencing side effects. My blood sugar has gone up a little bit, my memory (sometimes I forget things) and I don’t sleep as well as I did before.
I plan to share this with my Dr so perhaps he can make some adjustments. My question is my heart rate is now higher than it was when I do basic walking (low 80s to 90s) so I am erring on the cautious side given it is very soon from my event. I was cleared to do some very light resistance training and I don’t see much of an increase in HR so all good there. Prior to the event I would do a modified cross fit style work out and kept my HR in the 120-140 range with some pretty heavy weight lifting. I would spend time on the treadmill either as warm up / cool down & intervals several times a week.
I am expecting that given I am still doing a lot of healing inside so I should expect that my heart will be working a little harder now. In your experience how many weeks/months will it be before I will start to see my HR back to a more normal level when I am exercising / walking?
Thank you!
Hi Jeff,
You’re right to pay attention to the fact that there is still healing happening on the inside. At a glance, the meds you’re on are commonly prescribed right after an angioplasty/stent in order to prevent clotting (Brillinta in particular). You didn’t say which medication you’re on to control your HR and BP, but I’d imagine it’s probably a beta blocker like metaprolol. Beta blockers tend to reduce your resting and exercise heart rate, so if you’re finding that your HR is higher than it was before at an equivalent workload, you might want to speak with your doctor about this and get some feedback.
In answer to your question, in general, after a heart attack and angioplasty/stent procedure, usually after a couple months or so, most people tend to be doing quite well and getting back to normal. BUT, the most prudent course of action is to discuss your recovery time with your doctor because not everyone’s case is exactly the same. Given that you were active going into all this, that will certainly help you with getting back into your activity again. Once you get the final clearance from your cardiologist, then you should probably be able to work back up to the higher exercise intensities again.
Hope this helps. Kind regards, Bill
Thanks Bill! (yes on the exact beta blocker you noted. Yesterday I was cleared by my cardiologist with no restrictions. Yay! He wants to push it on a stress test in a couple of months but for now I can go back to weights, continue cardio. (clearly as you say I am still healing so I will be going slow.) He said that I said minimal damage (likened the heart muscle and arterial structure to a 30 acre forest and I damaged 2 branches off of 2 trees) So he expects me to pretty much be back to normal. By God’s grace I was able to get to the hospital in about 10 minutes after the event. Thank you for responding and for this wonderful website packed with information!
Hi Jeff,
I’m really glad to hear the good news. That’s a great analogy. I think people often think that a heart attack, any heart attack, is the end of the road, but if you get quick treatment and it just so happens to be a “small” heart attack, then you can recover quite well. I would also suggest asking your doctor what your ejection fraction is, as this will tell you how well your heart is pumping blood. In general, anything about 55% or above is desirable. When you get down in the 40s and 30%s or below, then that’s cause for concern. In the meantime, just be sure to keep on top of everything and get the exercise and rest your body needs during the recovery process. Kind regards, Bill
Hi Bill – it is 59.9% I am resting and doing the recovery process for sure! I noticed that hot weather has an effect given the beta blockers and that I am a little less than a month from my event. I am grateful for every new day – thank you again.
Jeff
Hi Doc
31 male. Weigh 100kg. 188cm tall.
Drink ocassionaly. Never smoked. Diet isnt great but not awfal compared to some.
Cholesterol checked and doc said its normal whatever that means.
3 weeks ago during rest. Doing report on computer i had pulling sensation in the centre of my chest. On 2 ocassions within 5 minutes. Followed by left arm feeling heavy and numb.
I went to hospital they done a heart trace and said it was normal. Done bloods and told me i didnt have heart attack. A few days later i completed a stress test with ecg connected. They told me it was a good test.
Doc treated me for imflammation of chest wall. Took meds for 2 weeks. During this time i have had sharp pains in left and right side of chest. Odd pull sensation in centre. On left side of neck and on left arm also had pains. Left hand goes numb during the night. Doctor told me yesterday to stop taking meds for imflammation because it doesnt seem like the issue. I always get these pains during rest not when im active.
I have a heart rate of 55 at rest. When i first wake up it can be as low as 44.
Please advise if any of this makes sense regarding potential heart issue.
Hi Kieran,
Thanks for your comment. Based on what you’ve written, it appears they did a resting and exercise electrocardiogram (which is where they put the electrodes on your chest) and checked your cardiac enzymes like troponin (which is an indicator of heart damage if you’ve had a heart attack). All of these results appear to be good news. Was there any talk about doing a cardiac catheterisation? The only issue with this is that it’s an invasive procedure, so docs are hesitant to do one of these unless the other things come back positive.
The fact that you’re NOT getting pain with exercise, but instead when you’re at rest which would be consistent with unstable angina (angina is just a fancy word for chest pain). Ultimately, you need to get to the root cause of what’s causing the chest pain. I would strongly suggest talking to your doc about the possibility of a vasospasm causing your symptoms. I’m not saying this IS what it is, but about 2% of people with angina (chest pain and pressure) have coronary artery spasm. It’s not totally implausible given all the other information you’ve provided. Hope this helps. Kind regards, Bill
Hey Doc
Thanks for the reply
I got a CT angiogram done of my heart and they found a fistula in coronary artery. No narrowing or blockages.
I am still waiting to hear from the cardiologist on the best way forward.
Looks like i had this from birth but was never picked up. Its took me 31 years to get symptoms.
Strange.
Just a nervous waiting game on how we proceed.
Hi Kieran,
Well, I’m not happy to hear they found the fistula in your artery, but the good news is, better the devil you know than the one you don’t. It’s better to have it caught and managed now than potentially cause problems later on down the road.
Dr. Sukala,
I am a 62 year old male, 6’ 3” 185 lbs. Resting pulse in the low 40s. BP unmedicated 140/85,
3 months ago two stents were put in my left anterior descending artery and a ballon was used in the circumflex artery.
The meds include Clopidogrel, children’s aspirin, Ramipril, and Rosuvstatin.
As a very long term elite long distance runner I was very surprised that a problem was found during an EKG. Over the course of about 2 years there has been a greatly diminished aerobic ability. None of the medical specialists knows for sure what my problem is. The stents have not changed the aerobic condition. I’ve seen otolaryngologists, respiratory specialists, a pulmonologist and cardiologists. I have taken my time getting back into running with no ill effects.
So is there a chance my heart blood supply is still being occluded? The stent area was 40 to 60% blocked. I would not have found this out until years later and much worse result if it were not for the poor aerobic ability that still evident.
Three years ago I also had a pulmonary embolism. Running was still good for a year after that. My relay race running team told me today to not be on the team this year. They don’t want to have a medical emergency in some remote area. Even though I have run hundreds of miles since the angioplasty perhaps they are right?
Hi Larry,
Thanks for sharing your story. I can empathise with your frustration given that you’re used to being really active and then this lands in your lap. In regards to your questions, I can’t give you medical advice but can probably give you some points to discuss with your medical team.
Regarding your heart blood supply, when they did your angiogram, they should have made an assessment of the arteries after the angioplasty and stent deployment. I would recommend speaking to your cardiologist for that information. As you rightfully pointed out, it’s a good thing they found this early because essentially you only had a plumbing problem rather than a heart problem.
Second, regarding your exclusion from the team, perhaps it would be worthwhile discussing with your doc the possibility of having a treadmill stress test done in order to check out your ticker at higher intensities. Based on what you’ve provided, you are clearly well-managed and if your stress test shows that you can tolerate some pretty grueling exercise, then this may convince your team mates to let you participate. You should also emphasise the point that you are already doing lots of running that far exceeds the distances you’d be running in the relay.
Hope this helps.
Kind regards
Bill
I recently had a heart attack due to a very high blood platelet count, which I didn’t even know I had (caused by the Jak-2 gene). The cardiologist inserted 2 stents. Prior to this I worked out (mainly lifted weights with 5-10 minutes of cardio) 3-4 times per week. I am not heavy (6′, 162 lbs.) don’t smoke or drink. I feel pretty good and was wondering if I should begin lifting lighter weights and doing some cardio again.
Thank you,
George
Hi George, Feeling good again is a good thing, but there might still be healing happening on the inside, so always best to speak to your doc about having a stress test done (when appropriate) and see if you’re able to tolerate high workloads on the treadmill. If the test results are uneventful (i.e., normal heart rate and blood pressure response), then ask your doc if weight training is appropriate and what intensities you should begin with. Always best to work with clinical data and your doc’s recommendations. Kind regards, Bill
Dr. Sukala,
Thanks for the advice. I will follow up with my doctors and racing team !
Dr. Sukala,
I know that you have a busy schedule, but I have a critical question
that I hope you can answer. At age 72, and a 58 year competitive
athlete in track (middle distances), I have been advised after a number
of different tests, to have a Angioplasty procedure, with the potential
of one or more stents. I am concerned about the post recovery, especially
as it pertains to my training. Everything I read refers to aerobic and
weight training, but not anaerobic. I train about 60 miles a week, with
two days of speed workouts (400, 600, 800 and 1200 meters), and am
wondering about the down time for speed work. I understand that
every case is different, and most doctors don’t like to speculate,
but I am scheduled for the procedure in two weeks, and need to have
some good estimate on returning to training, especially anaerobic
workouts. Your thoughts would be very much appreciated. By the
way, I hold a number of U.S. masters records, and in the 1980’s once
held the U.S. record for all men over 40 with a 4:15 mile, and am in
the USATF Masters Hall of Fame.
Thank you,
Harold J. Nolan, Jr., Ph.D., MBA
Hi Dr Nolan,
Thanks for taking the time to leave a comment here. Wow, you’re the real deal! I feel like I’m responding to running royalty!
I’ll say a few things here to bear in mind regarding the angioplasty procedure, subsequent recovery, and return to training.
First, from my experience, most people who are quite active and otherwise healthy going into an angioplasty/stent procedure tend to do quite well on the recovery side because 1) there is a high level of motivation and a desire to get better; and 2) the underlying fitness really helps facilitate the recovery. Someone who goes into an angiplasty/stent with 50+ years of bad habits and no underlying fitness foundation may find it harder to get “on the wagon” so to speak compared to someone with a lifetime of exercise under their belt.
Second, remember that after the procedure, even if you feel great, you are still healing on the inside. In other words, DO listen to your doctors and any recovery precautions. In most cases, people heal up just fine, but the times I’ve seen things go bad is when someone with Superman Syndrome goes out and overexerts themselves, leading to a sharp rise in heart rate and blood pressure. When they do an angioplasty, the docs are in there poking around with the catheter, inflating a balloon, and inserting a stent. So when it’s done, it’s important to be aware that those arteries are still sort of “settling down.” So while you might outwardly feel great, it’s important to ease off the accelerator a bit in the initial recovery period until you go back and see your cardiologist for a follow up appointment (usually about a month or so).
Third, regarding anaerobic exercise after an angioplasty, here are some things to consider that you might like to discuss with your doc. 1) Level with your cardiologist and inform him/her of your exercise history. You’re clearly in another category of exerciser, and the fact that you have a high level of underlying fitness will bode well for your case. 2) If you have a cardiac rehab program near you, get into it. In the US, they are more inclined towards using continuous telemetry monitoring during exercise so they will be able to see if there is anything happening on your ECG at higher workloads. If you’re tolerating reasonably high workloads with no ill effects, then 3) talk to your doctor about having a max treadmill stress test to see what your ticker is doing at extremely high workloads. If the ECG is unremarkable, then your doc may give you the green light to get back into your anaerobic training routine.
Fourth, remember that if you have NOT had a heart attack (which appears to be the case here), then you technically didn’t have a “heart problem” but instead just had a “plumbing problem.” Assuming the stents are all stable and all your vitals are within normal limits, then more than likely your doc will give you the green light. I think it’s important to point out that whether you’ve had angioplasty/stents or not, exercise carries inherent risks for anyone. In your case, better the devil you know than the one you DON’T know. The other thing is that exercise and training is a massive part of your life. If you can’t do this, then it MASSIVELY encroaches on your quality of life. I would imagine you have lots of team mates that you train with who are also close friends. So even with all the inherent risks associated with exercise, I’d imagine you’d deem it a risk worth taking given all the benefits to your health and social connectedness. Point is, be sure to point out the bigger picture in your talks with your doctors too.
In closing, I imagine that you’ll be just fine provided you 1) follow your doc’s advice; 2) go through the recovery process as recommended; 3) get into a cardiac rehab when approved by your doc; 4) have a TM stress test done when you can get it scheduled in; 5) Get back to training provided you’ve weighed out all the risks vs benefits.
Hope this helps.
Kind regards,
Bill
Dr. Sukala,
Thank you for taking the time to address my question about resuming
anaerobic exercise (speed work for track events) after a possible Stent
procedure. You advise is well received, as I gear up for this procedure.
I will be doing as you suggest in terms of working with my medical
team to be sure that I give enough time to things to adjust, and hope
to be part of the indoor track season next winter. Thanks again.
Harold J. Nolan, Jr., Ph.D., MBA
Hi Dr Nolan,
I’m sure you’re going to be fine. In general, those that do well after the procedure are the ones that follow their doc’s advice and go through the recovery as directed. Keep up the great work and I look forward to seeing more podium finishes from you!
Hi Bill,
I am a 55 yr old lifetime competitive cyclist, just under 2 weeks ago I had an Echo Stress test, where the Cardio, stopped 10 mins into it, no pain just shortness of breath, he didn’t like what he saw on the screen, also in the Echo afterwards where he saw some abnormalities.
When I had a chat with him afterwards he said he was pretty sure I have Coronary Artery disease and booked me in for an Angiogram.
I had the Angiogram last Monday, where they found a 50% blockage of the LAD, which they didn’t stent ( I understand why), they also found a chronic occlusion of the right coronary artery, which he didn’t stent. He now wants to do a more thorough Echo next Monday, to see where to go.
I have been doing some reading, do you know anything about CTO PCI’s, as I believe there is a Dr in Sydney who does it, but from what I read it is hard to PCI a completely blocked artery.
Anyway if you have anything you could help\advise me with it would be much appreciated.
Hi Tony,
Thanks for your comment. There are a few things to bear in mind in your case. First, the fact that you are a long time competitive cyclist may mean that you have developed collateral circulation around your blockages. I would suggest speaking with your doctor about this and ask him if he found any evidence of collaterals built up from your years of training. I have seen a number of people who were so fit from exercise that it masked their coronary artery disease.
You mention there was a 50% blockage of the LAD and an occlusion in the RCA. Did he give you a percentage on the RCA or is it 100% blocked? In general, docs tend to be less inclined to do an angioplasty/stent when it’s less than 70% (obviously this depends on the cardiologist and his/her clinical judgment in different situations).
Regarding the chronic total occlusion (CTO) percutaneous intervention (PCI), this will be one of those situations where you’ll have to discuss the risks versus benefits with your interventional cardiologist. If you are symptomatic (i.e., you’re having chest pain or shortness of breath at rest and during exercise) then there are quality of life issues, so a CTO PCI or a bypass surgery might be warranted. As I mentioned above, perhaps speak to your doctor about any collateral circulation which may have formed around the RCA. If your heart muscle served by the RCA is getting sufficient blood flow despite the blockage, then your doc might assume a wait and see approach. While collateral circulation may be sufficient at rest, it’s possible that it’s not enough when you’re exercising and therefore may warrant some sort of intervention (more on collaterals here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689049/). And since you’re a high level cyclist, symptoms during exercise would definitely impinge on your quality of life.
If you do need some sort of intervention (ideally only a PCI and not open heart surgery), the good news is that you found this now BEFORE you had a heart attack (which could cause heart muscle damage). You only have a “plumbing problem” at this stage but your heart muscle is fine.
I hope this was helpful for you. Obviously I can’t give any specific medical advice, but I can assure you that looking at the big picture, you have a lot of positive things going for you (i.e., regular exerciser, likely collateral circulation, blockages but no heart attack or heart muscle damage).
For here and now, I would try not to overthink it in any direction until you get your more thorough echocardiogram done next Monday. The more information you have on your heart, the better you and your cardiologist will be able to find the best course of action.
Feel free to stop back and leave an update with how you go, as this information may benefit other people out there going through the same thing.
Kind regards,
Bill
Hi Bill,
It’s a little over 12mths since my last post. A few weeks after I posted I had another angiogram done, this time it was an FFR of the LAD, where they found the flow rate was 0.87, still to low to stent according to my ‘cardio’.
I have still been cycling a lot and competing as he said it was ok to do, I even rode from Canberra to Qld sole in March to raise funds for SidsnKids, done this 4 times and raised nearly $35000.
Anyway I still am bothered by shortness of breath when I go hard on the bike, probably is a little worse.
I have been doing some reading and found an article from the AmericanCollege of Cardiology, referencing and European Cardio study, where they said that Masters athletes, especially endurance ones like cyclists were a lot different and sometimes the guidelines don’t allow for how hard they might push themselves during competition or training and that they may be more likely to need pci, than using the usual measurements.
Hope that makes sense. My Cardio has said to me that the stress test I did last year really did seem to point to the stenosis with the proximal LAD. He said he my consider stenting if I was still having SOB on exertion even though it was only 50%, BUT When I went back to him he said no he wouldn’t. So I am a little at a loss as to what to do. Maybe I need another opinion.
Thanks again in advance
Hi Tony,
Thanks for your comment. I can certainly empathise with your frustration, given that you’re a highly trained athlete and this is really cramping your style.
If you haven’t done so already, it may be worth your while bringing the ACC article to your cardiologist’s attention. As you point out that the stenosis is around 50% in your LAD, most cardiologists would be hesitant to do a PCI because there are always surgical risks. Chances are, you’d be just fine if they did do the PCI, but I think many cardiologists are risk-averse.
While I can’t tell you what you should do, you would be well within your rights to request another opinion, perhaps with a cardiologist who is also an elite athlete (they do exist out in the wild!). With that in mind, he/she might be more understanding to your dilemma.
The other option (which might not really be an option for you) is to moderate your intensity since you said it comes on at higher workloads. But then that would also impinge on your quality of life since you are accustomed to doing those high intensities.
By the way, congrats and kudos on your ride from Canberra to QLD. That’s quite a hike! And for a great cause too!
Hope this is helpful.
Kind regards,
Bill
@Dr Bill Sukala, Hi Bill,
Been meaning to contact you for a while, I had a second opinion with a different Cardiologist in Sydney, he looked at a CD copy of the angiogram I had done in Aug 2019, and said he thought the diagnosis didn’t look right, so he did another angiogram in early Dec 2020, and discovered that I did not have any blockages at all in my RCA, and a small 20% blockage of the LAD
He could not beleive how incompetent my Canberra Cardiologist was.
He also said he is very worried about my worsoneing SOB, and also couldn’t beleive I was given the ok to keep competing on the bike.
So to cut a long story short, I have had a heap of tests since Xmas and after a Cardiac MRI, looks like I have Cardiomypathy, ie; damage to the Myocardium, from a virus, most likely years ago, showed up as a LGE, which apparently points to this.
On drugs now to try and get my LVEF up, otherwise will considered for prophylactic ICD therapy, which is bit scary.
So that’s where I am at.
cheers
Tony
Hi Tony,
Thanks for getting back to me with the update. I imagine you must be a bit frustrated after all you’ve been through. Looks like a lot going on, but sometimes still better the enemy you know than the one you don’t. Let me know how you get on with the ICD. Warm regards, Bill
Hello Dr. Bill,
Thank you for the informative post.
I am 36 years old and have been an athlete most of my life. I don’t smoke and my diet is mediocre. I have familial coronary artery disease and hypercholesterolemia. About a year ago I started feeling chest pain when exerting effort at the gym. It would happen once every 2 weeks so I thought it was a muscle spasm but later I started feeling the pain every time i increase effort.
Did an angioplasty and the doctors decided I needed open heart bypass surgery which I underwent in January 2019 (LIMA to LAD and SVG to OM1-OM2 sequentially). By April I was back at the gym mostly on the bike and treadmill and by June I was lifting light weights and increased the intensity of my cardio workouts while feeling perfectly fine.
I travelled in mid July and was walking (far less intense than my gym workouts) an average of 8 miles a day and suddenly I started feeling a slight anginal pain. Not quite like the pain before my open heart surgery but I could feel something was wrong.
I did a cardia CT angiogram and turns out there was stenosis in my SVG vein graft in 2 locations. Two weeks ago (August 26th) My doctor performed angioplasty and inserted 2 stents to open the vein.
Thankfully I haven’t had a heart attack and the heart muscle is in excellent condition.
I’m struggling with anxiety and have panic attacks which doesn’t make things easy because as you know the symptoms are similar to heart attacks. I’ve been having chest tightness and pain and have been to the ER 3 times to do ekg and Troponin t tests. It’s that bad.
My question is when can I go back to walking up stairs, slight uphills or even lifting light weights. I’m afraid to do any of that after having stents placed (more so than when I had CABG!!). I feel paralyzed.
I’m currently walking 25 mins on a level surface twice per day without issues.
I’m currently on the following medication:
Crestor 20mg
Repatha 140mg
Concor 2.5mg
Brilinta 90mg
Aspirin 81mg
Nexium 40mg
And I carry my nitroglycerin spray with me at all times.
Sorry for the long message and thank you for your time
Hi Zaid,
I’m sorry to hear you’re having a difficult time with everything after your surgery and angioplasty. It’s certainly normal for you to feel a bit of anxiety having gone through all that. One of the best things you can do at this stage would be to seek a referral to a psychologist/counsellor who is trained in helping people who’ve gone through some serious medical issues. He/she can help you work through some of the thoughts and feelings you’re having and give you more peace of mind. Remember that reaching out for help is a sign of strength and not weakness.
Provided that your saphenous vein grafts are clear and you have clearance from your doctor to exercise again, then it will just be a case of gradually increasing your distances and intensities so that you can get “reacquainted” with your body now in the post-surgery stage.
To your credit, you’re very smart to be paying close attention to your symptoms. Plus you’re on the better side of the equation given that your heart muscle is still in good shape.
Again, I think the best thing right now is to seek out a psychologist/counsellor/social worker with experience in helping people after medical events. I can assure you this will really help put you on a good path back towards health. Anxiety is no fun but you can definitely control it with cognitive behavioural therapy (CBT) techniques.
Feel free to leave another comment here if you have any other questions.
Kind regards,
Bill
I love this article and must of read it 3 times. I am a 60 year old male. Never smoked, maybe 20 pounds over weight.
6 weeks ago I had four stents inserted. Never had heart attack. I have one other minor vessel located lower left that is blocked but the Dr was not concern about it so left it be.
I am on Ibersartan 150 mg and have been for 15 years.
Rosuvastatin 40 mg, was 10mg for 25 years
Ticagrelar 90 mg
Baby aspirin.
Now after my surgery, they put me on Metropolol at 37.5 mg twice per day to lower my heart rate.
After 10 days due to side effects and feeling crappy they lowered to 25 mg twice per day. Again my new normal heart rate was below 55 bpm and I am still feeling crappy. Light headed, zoned out, sissy. Sometime my BPM drop to below 50 bpm.
So dropped to 17.50mg twice per day. Still crappy feeling.
Gave up on that and now I am on Bisoprolol at 2.50 mg once per day.
I can go for good walks, lift weights and jog hard for one minute with no discomfort or chess pain.
However I still feel crappy at times. One night I went to bed feeling good and five minutes later I was having chest pain and landed up taking one shot of nitro and this relived the pain and I fell asleep.
Now my heart rate is about 65.
What should my at rest heart rate be?
Should I be having chess pain? At rest?
Or do I just need to give this all time and be patient and let my body heal and get use to the new meds. Help.
From tired of feeling crappy.
Thank you
Hi Allan,
Thanks for your comment. First off, the good news is that you were able to catch the blockages early and get treatment so, as you pointed out, you do not have any compromised heart muscle.
As for beta blockers, yes, they can really knock the stuffing out of you and make you feel really tired. They affect people differently with some people being very sensitive to them and others able to tolerate them reasonably well.
I would suggest speaking to your doctor in greater detail about the meds you’re on and mention that it is impinging on your quality of life. Usually there are other options available in terms of meds and dosages which can help but without all the side effects.
As for your resting heart rate, in general, beta blockers will tend to slow down your resting and exercising heart rates. The textbook “normal” resting heart rate is, on average, between 60 and 100 beats per minute. But if you’re down in the 50s then that’s nothing too far out there. Everyone’s hearts are wired a little differently, where some people are around 45 at rest and others are 90 bpm at rest. It’s not to say one is necessarily healthier than the other, but just that the electrical innervation of the ticker is wired a bit differently.
If you’re having chest pain at rest, then this is something that would be worth discussing with your doctor. In general, you shouldn’t be having chest pain at rest. It may be nothing, but just to be sure, it’s best to get checked out to be sure.
Feel free to stop back and leave another comment if you have any other questions or concerns.
Hope this helps.
Kind regards,
Bill
Hello Dr.
I have a few questions I think you may be able to answer for me. First let me tell you a bit about myself. I am 55 and worked in construction since I was 16, building new homes, heavy lifting of lumber and climbing around on roofs.ie very active for 8-10 hrs a day. 5 yrs ago I was offered a PM position for a large construction company in which I took the position. I am an ex smoker- on 15yrs off for 10 yrs back on for 10 and now off again for the last 7yrs. I was having some breathing problems 2 years ago and after seeing a few doctors I ended up seeing a pulmonologist who diagnosed me with chronic asthmatic bronchitis in which I use an inhaler, (Symbicort)2 puffs twice a day. Also my weight has been fluctuating from 190 up to 235 and then back down to 205. The weight fluctuating I did on my own because I would diet for a while then I will go off and then I will go back on and it seems (which would be obvious )that when I am heavier the breathing problem would accelerate when climbing stairs etc. I don’t do the heavy work anymore since I became a PM. My PCP recommended that I see a cardiologist to discuss my breathing issues because my pulmonologist said my breathing issues are not that severe because of my weight fluctuations. My cardiologist recommended an exercise stress test (Treadmill) I did 85% until my calves and thighs cramped up and I could not finish because I am out of shape from being out of the construction for the last five years. I feel fine though physically now unless I push myself to do things I wouldn’t normally do as stated earlier climbing 5 flights of stairs or walking for more than 45 minutes in which I do a lot of in my new position as PM. Trying to make a long story short I was told from my cardiologist I had ST Depression in my stress test so now he’s recommending cardiac catheterization to see if there are any blockages. I also forgot to mention earlier that my blood pressure is perfect and has always been my whole life. One of my questions is from your professional opinion do you think that the cardiac catheterization is necessary. The reason why I’m asking is because I am supposed to get Umbilical Hernia surgery in the next few weeks , I’ve had the hernia for many many years but it never bothered me and now it is . My cardiologist had said if I get any type of angioplasty or stent that I cannot get the hernia surgery for quite some time but it is critical for me to get the surgery because it is getting worse and can become strangulated. I feel like I’m between a rock and a hard place I don’t know what to do first. My Surgeons will not do the surgery until I am cleared from my cardiologist. I just feel that the cardiac catheterization is not necessary, is there something else or another type of test that can be done that’s not so evasive and can conclude if I have any blockages. I would also like to mention that I had a Trans thoracic Echocardiography-TTE before the exercise stress test that my cardiologist recommended I take and it came back 100% normal. I just feel that the cardiac catheterization is not necessary as I said earlier. Do you have any suggestions or input that I can jog around in my head and think about. I just bought a home gym prior to this happening and have not been able to use it yet since my hernia started to bother me. I am just very frustrated over the whole situation. I had purchased the gym because I wanted to lose weight again and get back into shape as I was when I was doing carpentry. Please, any advice would be appreciated. Thank you in advance. PS- If you’d like to email me in regards to this that would be much appreciated. Thanks again.
Hi Joseph,
Thanks for your comment. While I can’t give you any specific advice, I could suggest things you might like to talk about with your doctors.
Regarding the ST depression on the exercise stress test, this is basically an indicator that there “could” be some blockages in your arteries. Because ST depression is only suggestive and not conclusive, that’s why they’re eyeing up the catheterisation in order to get a closer look.
I wouldn’t necessarily say that the catheterisation is useless because comparing your heart to your hernia in terms of importance, your heart is always going to take precedence over the hernia. I know the hernia is not comfortable, but it’s true that your heart is going to be the main health factor calling the shots.
The docs who could do the hernia surgery are bound by ethics and protocols not to do the surgery until your heart is deemed clear and not a risk factor for the hernia surgery.
Remember that if they do the catheterisation, it’s possible they’ll find everything is normal and may not need to do the angioplasty.
From here, I would suggest getting more information on how long you’d have to wait for the hernia surgery IF they did the angioplasty. In general, most people return to their normal activities of daily living within a couple weeks, and by one month, most are cleared by their doctor to go about their lives as before the procedure (i.e., doing exercise etc).
Knowledge is your best friend at this point, so best to get all the information now and then look at all options (i.e., if you need the angioplasty, how long til you can do the hernia repair? Or if no angioplasty needed, then can you do the hernia repair asap?). There are a few moving parts here but again, I’d recommend working closely with your medical team and discussing your concerns in hopes of finding the best outcome.
Sorry I can’t tell you what to do, but I hope some of this helps give you some things to discuss with your docs. Hang in there and feel free to stop back and leave another comment if you have any further questions or comments.
Kind regards,
Bill
Hello again Dr.
First off I’d like to say thank you for the quick response. I ended up having the angioplasty 2 days after my last post, and after my complaints about it being unnecessary to my surprise ( man was I wrong) I ended up having 3 blockages. My discharge papers say, and I quote- ” Your provider diagnosed you with :3- vessel CAD”
” Your doctor performed the following procedures: Percutaneous coronary intervention (PCI) with insertion of stent into left anterior descending (LAD) coronary artery”- end quote. So it turns out, out of the three blockages one I was told basically healed itself I don’t know the exact medical terms for it but the doctor explained that it found another route, in essence it did its own bypass. The second blockage was not considered enough for a stent at this time, but they may want to do a radiation stress test in about 6 months, and the other one had stents put in.. That was my update to my last post.
I now have some new questions maybe you can answer I seem to get a better response from you than from my doctors, seems like they’re always in a hurry, nothing personal against them but I guess they’re just busy. First thing I would like to add is during the procedure while I lay on the table in twilight zone my doctor said to me Quote’ “Joseph you have three blockages, we can do stents now or we can arrange to do bypass surgery, if we do the stents you won’t be able to get your hernia surgery for at least a year” end quote. I wish this was discussed before I was on the table if there were blockages being I wasn’t in my right mind at the time to make that decision and obviously I opted for the stents and I’m not sure if I made the correct decision because from what I read the bypass is actually better than the stents and without needing long-term medications which will affect my future for any surgeries or even dental work. So anyway what’s done is done and can’t really turn back now. My questions are the medications that I’m on.I was prescribed Prasugrel 10mg one a day, Aspirin 81 mg EC, once a day, Metoprolol ER 25 mg once a day, and they raised my Lipitor at which I’ve been taking for over a year from 20mg to 40mg a day. Since then I’ve been having severe ringing in my ears and I contacted my doctor in regards to this and he told me to stop taking the Metoprolol so I tried that for a few days and the ringing is still severe. When I contacted him again he said go back to 20 mg Lipitor and continue the Metoprolol. My questions really all about the medications, is the Metprolol in your opinion necessary for my conditions because I heard bad things about beta blockers and it seems he was very quick to say stop taking it . I don’t have high blood pressure I did not have a heart attack and I did not have angina I’d rather not take the beta blocker. I’m not going to use your answer as my one and only solution I’m just asking your opinion from your past as being a doctor and dealing with other patients.
I was told this yesterday from my doctor but I have not started yet I am still taking the 40 mg Lipitor because I really would like to find out if I need the beta blocker.
I really appreciate your opinions and comments. Thank you
Hi Joseph,
Wow, you’ve been through a lot recently. Hang in there because the early post-op days are usually a bit of an adjustment. If you’re feeling pretty wonky then rest assured that’s not uncommon. It’s not fun, I know, but it’s also not uncommon after they’ve been poking and prodding around your coronary arteries (congratulations, you’re human).
Regarding your meds, as I’ve said before, I absolutely cannot give any yes/no sorts of answers since 1) I’ve got a PhD not a medical degree; and 2) you’re not under my care. So having said that, the combination of meds that you’re on are pretty much standard after an angioplasty/stent procedure, independent of whether or not you have high bloodpressure. As you noticed, a beta blocker (metoprolol) can really sap you of energy, so I would suggest forcing the issue with your docs and have another conversation about the symptoms you’re having and discuss if there is more leeway for you to request a reduction in meds or a shift to something else, as appropriate.
I apologise that I can’t be more specific. The reality is that everyone is a bit different and docs tend to make their decisions based on your unique clinical picture. What’s right for you might not be right for someone else who brings other things to the table, and vice-versa.
I would suggest hanging in there as best you can and usually by around a month or two, you should be feeling much better. The early post-op days tend to be the roughest for most people. Hope this helps.
Kind regards,
Bill
Hi there, thanks for publishing a ‘real life’ article that actually answers some questions, I wonder if you might have a view on my situation? I’m 59 I had a stent to resolve a 95% blockage in my LDA in January and was previously pretty fit, the only symptoms I ever experienced pre-stent was a tiny amount of change in my breathing when going from nothing to something exercise wise, a few years ago I could run 2 marathons a week but owing to injury my fitness had definitely declined although in the weeks prior to the stent i was mountain climbing in the Canary Islands. Since the stent I have lost a decent amount of weight and taken up running again, I have entered a marathon and altered my diet to remove sugar, grains and wheat and dairy products (what’s left can be a bit boring 🙁 ) and I generally feel much better, I’m finding raising my training distances increase my max heart rate to around 150 – 170 depending on gradient of the surface and this begins to affect my CV, I had the results of an ECHO recently that showed my left ventricle was pumping about 10% down from normal which is thought to be contributing to this limitation I’m wondering if running, and the resultant increase in heart rate might, which during a marathon can be for extended periods, might actually be causing damage to the heart muscle, rather than improving it? I can walk run which brings my heart rate down whilst walking but the increase is pretty immediate once I start to run again. I’d really appreciate any general advice you might be able to give.
Hi Colin,
Thanks for your message. I’ll say a couple things to preface my response. First, I changed your last name to your last initial just to protect your privacy. Second thing, I can provide a few observations and things that you might wish to discuss with your cardiologist, but I don’t give any specific advice as in, “do this, do that.” With that said…
The first thing I notice is that you’re a pretty fit guy. I think you likely have a lot of collateral circulation built up in your heart which was compensating for the blockages. This is very common in athletes and can mask symptoms until much later (which appears to be your case).
Regarding your compromised ejection fraction, I would suggest you ask your doctor the reason for this. Did you have a heart attack as well? Usually a small drop in ejection fraction can be due to a little bit of heart muscle damage after a heart attack. I’m not saying you had a heart attack though, but definitely something to discuss with your doctor.
I can’t say that exercise would be causing any damage to your heart, unless there was a specific contraindication by which exercise would worsen your condition. I’d say this is unlikely but perhaps worth talk to your doc about this.
One thing to remember is that exercise has benefits not only for the heart muscle itself but also the rest of the body (what we call peripheral changes). I’ve seen people with very serious congestive heart failure who were, astonishingly, quite tolerant to some pretty gruelling exercise. One guy in particular, I recall he had an ejection fraction around 30% or so and yet he was still a competing cyclist. In his case, the rest of his body was so fit at extracting oxygen and nutrients from whatever blood his compromised heart was pumping that he was still able to train and compete. I wouldn’t say he was the norm, but he was willing to keep going no matter what.
In your case, I would imagine that you also have a lot of peripheral adaptations which are protecting you and helping out your heart.
Moving forward, I would first recommend speaking to your doctor and making sure there are not reasons that exercise would be harmful to you (unlikely). Specifically, ask him/her if there are any contraindications that could make exercise dangerous for you.
You might also request a stress test to see how everything looks on the electrocardiogram. Assuming that at high workloads everything is working well, no blips or squiggles out of place on your ECG, no signs or symptoms, then that’s a good sign that you’re able to tolerate high workloads and with reasonably low risk.
If you’re prescribed medications, they can also tend to knock the stuffing out of you, beta blockers in particular. So be sure you understand all your meds, the effects they have on you, and how they might influence your exercise prescription.
Finally, as I mentioned above, try to get to the bottom of why your EF% is 10% down from normal and what might be causing that. Ask if it looks to be permanent or would it recover some.
You might also see about visiting a clinical exercise physiologist in your area. Based on your IP address, you appear to be located in London or near there. I would suggest getting in touch with the British Association of Sport and Exercise Sciences (https://www.bases.org.uk) and ask them to help you locate a qualified EP with experience working with people with cardiac problems. I’m sure it will really help give you some clarity and peace of mind.
Hope this helps you sort out some of the things in your mind. Any questions, feel free to stop back.
Kind regards,
Bill
Hello Dr Bill,
I’ve been reading your comments and must say its of great help.
Am 33 years old and recently diagnosed with Coronary Artery disease. No family history no previous symptoms. LAD 90% block, one stent placed. Everything else is clear.
This started with a pain above my left underarm accompanied with burping. I thought this would be indigestion but subsequent tests showed that there was a block. I don’t smoke and hit the gym 3 times a week. Overweight by a few kilos but i have lost a fair bit of body fat %. The doctor was surprised to see that i had a 90% block and was working out without any problems.
I had my Angioplasty on Oct 15th. Follow up ECG after 2 weeks, everything was normal. Dr’s gave me the green light to exercise. Am back at the Gym ( i rested for two weeks with no activity and gradually increasing since i have started) no pain while working out. Dr’s asked me to keep my heat rate at 70 to 80% of Max Heart Rate.
My question, since am very paranoid, is, will these workouts cause any problems to the stent. Any muscle pain on the left side also seems like heart pain :). Do advise.
Thanks,
Rahul
Hi Rahul,
You’re just a little bit over a month post-op now and you’ve been given the all-clear by your doctor. So chances are the stent is now set in place and the probability of having problems with the stent would be quite low. If you want to be extra careful, you can just make sure to take it easy for the next month to be sure. But if your cardiologist checked you out and gave you the green light, you should be ok.
Moving forward, you just need to be conscientious and aware of any symptoms you have. In general, if you have pain that is not going away no matter what position you’re in, then you might want to get that checked out. Often, if you have pain and you can relieve it by changing positions, then that is indicative that it could just be muscle soreness associated with your exercise routine.
Given that you are still quite young and are otherwise healthy aside from the surprise blocked artery, you would be relatively lower risk than someone with multiple blockages and lots of risk factors (i.e., smoker, high blood pressure, obese, diabetes, etc).
Bottom line: if in doubt, get in touch with your doctor or his/her medical management team (i.e., practice nurse) and let them know your concerns. They’ll be most familiar with your situation and can advise you on the best course of action.
Hope this helps.
Kind regards,
Bill
Thank you very much for taking the time to reply. If the pain continues, i will go and check this out before my next stress test which scheduled for Jan.
Thanks,
Rahul
Dear Dr Bill
I am glad I found this site due to the excellent questions & answers. There is nothing worse than being unsure of your capabilities & limitations.
I was a seaman working off Scotland in the North Sea. After working on the deck of a supply vessel I started to feel out of breath & dizzy. I called the Captain on the radio & told him about the situation. I knew I was having a heart attack due to previous medical training. Luckily the ship was only 50 miles from Aberdeen & a helicopter airlifted me to the infirmary. The crew did a great job keeping me stable with on-board meds & O2. About 1.5 hours later I was fitted with 2 stents initially on the 19th April 2019 then 1 futher stent fitted on the 23rd April. I was disharged on the 25th April & flew home to Croatia on the 28th April. I have done 2 weeks Cardiac rehab in Thalassotherapia, Opatija near were I live. It was fantastic & during my stay I had ergometry fitness tests, blood test & ultra sound. I’ve just had the 2nd tests done after 6 months & all is fine, very little damage to the heart. I was fit prior to the attack & now I am training daily, mostly walking & running with my dog, about 10-12 km tracks, in all weather, we love it. I also go to the gym in my house & do HIT with light dumbells everything seems fine. The problem I have is the Seafarering Doctor will not give me a Medical without restrictions and I cannot work as yet. My job is off the coast of Scotland supplying platforms & rigs so there can be rough seas & cold weather. Will I ever be able to go back to this job? I am finding it hard not to work as I am only 55 years. I have been at sea most of my life, military & merchant. I am now vegan, stopped smoking since the attack & feel fit & strong. I have another 4 months of medicines according to my discharge papers then just the statin & aspirin for life. What do you think. Looking forward to your reply.
Hi Keith,
Thanks for taking the time to leave a comment and share your story. There are a few things I noticed that I think would help you make a compelling case to get your medical release to return to work.
First, you did everything exactly right. You had cardiac symptoms that you recognised and you knew to get treated as soon as possible. Time is heart muscle and every minute is critical.
Second, they did the angioplasty, so it’s not like you were having symptoms and they decided to NOT intervene.
Third, you went to cardiac rehab and, by the sounds of it, you did really well with the program.
Fourth, you went back and had follow-up tests to ensure that your heart and the angioplasty/stents were fine.
Fifth, you’re active now on a daily basis which, by my estimates, might even be more physically demanding than the work you might be doing on the supply platforms/rigs.
Sixth, you’re only 55 years of age which is not “too old” by any stretch of the imagination.
Seventh, you’ve completely overhauled your diet and lifestyle which will further protect you moving forward and significantly decrease your risk of having another heart attack or need for another angioplasty/stent.
I can’t speak for the seafaring doctor but, strictly from an exercise physiologist’s perspective, you are clearly stable and medically managed. I think to add strength to your case, you might want to highlight your stress test results to the doctor and point out that you ARE able to handle some pretty gruelling activity (perhaps more than the job demands require).
I would also ask your cardiologist what your ejection fraction (EF%) is. Heart attacks can cause damage to the heart muscle, so doctors will often look to see how much blood the heart is able to pump out with each beat and also look for any heart wall motion abnormalities. If your EF is 55% or higher, then that’s normal (normal ejection fraction is between 55% to 70%).
Bottom line:
I would recommend having another conversation with the seafaring doctor and point out that you tick all the boxes for being medically stable and well-managed. If anything, your “volcano” already erupted and it’s a case of “better the devil you know than the one you don’t.” I’m sure there are other guys on the rigs with poor lifestyles and all the risk factors for a major heart attack yet, because they haven’t had anything happen yet, they let them keep on working. I’m actually MORE concerned about those guys being a risk than I am you.
Hope this helps.
Kind regards,
Bill
Thanks for the detailed advice. I recently had a heart attack after running a 5k ParkRun. I have run about 25 marathons and 2 ultras of 33 and 35 miles respectively. I am 1 month away from my 70th birthday. On the run I felt a pain in my upper chest and on completing (in 24 min) I had to go to the Emergency Dept. and eventually had a stent inserted into my left anterior descending artery. I was told that there was no damage to my heart and my heart returned to sinus rhythm after 3 days. I have been running for 51 years and wondered about my running future. Thanks for the advice
Hi Geoff,
Thanks for your message. You were smart to get attended to as soon as possible. Time is heart muscle. To your advantage, you did not have any damage to your heart muscle so, in effect, you had a plumbing problem rather than a “heart problem.” In order to get back into your routine, I would encourage you to get into a cardiac rehab if there is one near you and have them check out your heart on an electrocardiogram while you’re exercising. After you’ve had a month or two of recovery (and cardiac rehab), you might want to see if your doctor will do a stress test on you to see how your heart goes at higher intensities. If there are no signs, symptoms, or abnormalities on the ECG, then more than likely you should be able to get back to your running. Best bet is to have a good heart to heart conversation with your cardiologist (pun intended), and make sure he/she knows how important running is to you. Yes, there are risks, but the reality it, you were a higher risk before your heart attack. Now that you’ve had the stent inserted, it’s a case of “better the devil you know than the one you don’t.” You’ll know to be on high alert for any early warning signs and know to stop exercising if you’re feeling any symptoms. Assuming all your other arteries are ok and your stented artery remains patent (open and stable), then there is no good reason why you should be having any further symptoms.
Hope this helps. Happy holidays.
Cheers
Bill
Hi again Bill,
At the stage I initially wrote to you about 2 weeks after the event I didn’t realize that that the term for what I actually had was a cardiac arrest. My LAD artery was completely blocked and I my heart was completely stopped for 9 minutes before it was restarted. All the other details I told you about were correct. I went to a cardiac rehab course at the local hospital and did the stress tests, and after the course the cardiologist told me that I shouldn’t start running until 6 months after the event. 6 months have now passed. I have been walking every day, between 5 and 11 km, mostly up a hill as I was told to get my heart rate up to around 100 bpm. I was told that my max should be 114 bpm. I have cycled 20 miles on 2 occasions where my heart rate stayed below 114 bpm. Am I ready to start some jogging and slowly build up to steady running?
Hi Geoff,
Assuming you’re medically stable, have clearance from your cardiologist, and are tolerating exercise well, it seems feasible to start safely integrating a bit of jogging and running into your routine. It sounds like you have some guidance regarding your heart rate, so as long as you’re keeping vigilant and paying attention to any signs or symptoms (if any at all), then you should be ok. Feel free to stop back and leave another comment if you have any questions.
Cheers,
Bill
I had a heart attack with stent installed 2 weeks ago. I am 53 years old and in top physical condition (lifting heavy weights, run, play sports, active work) but have a family history of heart disease. I plan on taking it easy at first but wanted to know how long before I can begin lifting weights and running? I see my cardiologist for a follow-up next week and will ask him same questions. Just curious how you feel.
Hi Peter,
Thanks for your comment. Sorry to hear you had to go through all this but there are a number of positives working in your favour. First, the fact that you lead an active lifestyle more than likely prolonged the time until you had the heart attack. Second, your fitness level will certainly play a role in helping you get back on track with your routine. Third, while I’m not happy to hear you had a heart attack, at least now it’s better the devil you know than the one you DON’T know.
There is no cookie cutter recommendation for how long until you can lift weights and do cardio, but there are general guidelines that need to be considered on a case by case basis. In the immediate post-operative phase, you have to remember that there is healing happening on the inside (even if you feel well). So it’s important not to get your heart rate and blood pressure up too soon (at least a couple weeks or so). You can do what are known as “activities of daily living” so long as it’s not anything excessively strenuous. Once you’ve been back to your cardiologist for a follow-up appointment, you’ll likely get clearance to ease back into exercise. Rather than re-write my article here, spend some time reading the exercise section of this article and it will give you some guidelines to get back into it on the right track.
Bottom line:
1) make sure you’re deemed medically stable by your doctor;
2) get clearance from your doctor to begin exercise again;
3) pay attention to any signs or symptoms moving forward. If anything feels off, get it checked out;
4) ease back into exercise. Even if you feel like you can do more, err on the side of caution and gradually work back up to higher intensities;
5) go for your scheduled periodic check-ups with your cardiologist;
If you do all those things then chances are you’ll be fine. As I said above, it’s better the devil you know than the one you don’t know. And if you put safeguards in place then you can get things taken care of before they go from bad to worse. Hope this helps.
Kind regards,
Bill
Very informative well researched and extremely helpful post. It has made me immensely knowledgable with the subject. Would like to more about the exercise which can be done on treadmill after having angioplasty three years ago and when the health parameters are fine except the blood sugar levels are little on higher side which I think is due to lack of exercise. Kind regards. Sanjai
Hi Dr. Bill,
Thank you for hosting this page, and all of your super thoughtful responses. In my case, I am a 61 year young man, who is an avid life athlete and 6 time Ironman finisher, including Hawaii! About month ago, I was having trouble with my workouts. Rewind 3 weeks, and I failed a stress test and wound with up 95% blockage in my “widow maker” artery. Crazy! I got stented and am now experiencing unusual symptoms. My body felt like it was “adjusting” to the new stent for a good 8 days or so. I would occasionally get tremors, but no fever. This went away and I would have some good days, and go for an easy hour ride, but would feel them again later in the day. I tried skiing yesterday for 3 hours, and just felt tired at the end. And had more tremors. Today I feel just a little drained. Taking the day off. I read your guidelines to easing back in, and wish I had seen this article before. My meds are aspirin, Prasugrel, Resovustatin, and Omeprezole. Is what I am feeling normal? Is it from the meds? Just over doing it a bit? Its how I am wired so its tough to hang low. Based on your experience, when does this really pass so that I can resume my usual crazy ways? Thanks so much for your straightforward down to earth plain English responses! All the best -Jim
Hi Jim,
Thanks for taking the time to leave a comment and for sharing your story.
I guess the first thing to remember, and this goes for everyone, no two people are identical and it’s not uncommon for different people to have different experiences to the same procedure. I’ve seen people who’ve been through angioplasty/stent and didn’t have any untoward effects. I’ve also seen others like yourself that have had quirky after effects. In many cases, assuming your doc is aware of it and has cleared you, these things can tend to pass on their own. Remember that sticking a catheter up into your coronary arteries is anything but “normal” to your heart. It doesn’t like getting poked and prodded and, in some cases, there can be a localised internal irritation which could plausibly lead to symptoms as you describe. It’s not comfortable, but at the same time, neither is walking around with 95% blockage in your left main artery!
The first port of call should always be your cardiologist (or anyone else on the team directly involved in your care). They’ll be most familiar with your medical history and can probably provide you with a more specific explanation. Ideally, you’ll want to speak with the cardiologist that did the intervention (in case you have a different cardiologist that managing your after care) who, if he/she had difficulty during the procedure, maybe they’ll be able to give you a logical explanation.
As for your exercise, I always joke around with my athlete friends (and myself also being quite active) that athletes are THE WORST patients because your normal state is to ALWAYS be active and exercising. So when you have something go wrong with your heart or you have a musculoskeletal injury, you DO need to rest and let some healing happen on the inside. Unfortunately, the athlete’s brain doesn’t like to take no for an answer and we can be reluctant to heed the good advice to S-L-O-W D-O-W-N!
To be fair, there is a possibility the meds could have side effects, but again, it’s important to speak to your doc about all these things. As you’ve seen me say in many of my responses, I’m an exercise physiologist and it’s beyond my scope of practice to be able to comment on something that is ultimately the domain of your cardiologist. So the most I can do is at least give you some talking points which you should discuss with your doc.
In general though, it’s always good advice to just give it at least a month post-stent to cool your jets and let the healing happen on the inside. Yes, stay active, but don’t go red-lining it full throttle while your coronary artery is trying to heal and adapt to the stent.
Hope this helps.
Kind regards,
Bill
I received a saphenous vein bypass in 2004. In 2020 it became obstructed and was stented with a Boston Scientific Synergy. Actually two of them back to back, 3mm and 2mm. My cardiologist said my original artery was 98% obstructed. The rub is the bypass was to my inferior circumflex. It does not show up on a 12 lead ecg and was missed even with me on a treadmill with a Board Certified Cardiologist. What saved me was pain sending me to the ER and a 2nd Troponin test in the wee hours. They were going to send me home but offered me a chance to stay. So I doubt if any subsequent ecg is going to show much which means SWAG or nuclear perfusion treadmill. Or, just see how I feel. I used to XC ski. Now the general published advice is NO. Hardly do anything when it is colder than 40F. This is making me miserable and with Covid still rampaging, I don’t want to go to a gym. I know how to dress warmly. I am glad to be “ok” but I hate this and I hate being in a sedentary, inside quandry. Any thoughts?
Hi Mark,
Thanks for your comment and sorry to hear you’re having a rough go of things. Yeah, coronary arteries don’t always play by the rules and that’s one of those tricky things that sometimes they have to figure out what’s happening by other means. Most importantly, for right here and now, it’s been sorted out. It’ll just be a case of ongoing monitoring for signs and symptoms.
Regarding exercise, I can certainly understand how frustrating it is being physically active and not being able to do anything. Active people always have it harder when they’re injured or forced out of commission for a while (thanks for nothing COVID!).
I would recommend looking for alternatives like setting up a home or garage gym (either at your home or at someone else’s place). At least you could control the climate a bit to mitigate the cold and keep the temperature more stable.
If you’re interested in exercising outdoors, I would recommend speaking to your cardiologist and associated medical management team (i.e., practice nurse etc) and see if you can get any additional information specific to your situation that might allow you to exercise outdoors. It’s ultimately a case of balancing/minimising risk vs potential gains. In other words, the conversation you need to have is, if you’re otherwise reasonably fit, can you exercise safely. If the alternative is sitting at home doing nothing, then a sedentary lifestyle also carries its own risks. So what’s worse? Exercising in the cold (with precautions taken) or the potential health detriments associated doing nothing. I think if you can have that conversation with your cardiologist then perhaps you can find some middle ground.
Hang in there and feel free to stop back any time and leave another comment.
Kind regards,
Bill
Hi all,
I had a heart attack 4 years ago and have a pipeline of 6 stents in one artery.
I feel fine running and am running nearly as fast as before my heart event and am not sure if I should be trying harder. My cardiologist previously said to do what I did before heart attack.
Any thoughts would be appreciated.
Jim
Hi Jim,
Good to hear you’re feeling well. If you had the heart attack and stents six years ago and are medically stable and with clearance from your cardiologist, then you should be ok. The most important thing is to be aware and monitor yourself for signs and symptoms. If you notice anything a bit suspect, then be sure to get it checked out. In most cases, you’ll have symptoms before anything major happens. Good luck with everything!
Kind regards, Bill
Hi Doctor
I have had my stents put on 17th NOv 2020, It has been six months yesterday.
Age 61
wt 61 kg
ht.176 cm
I have lost 12 kg in six months. could it be due to statins . I was taking 10 mg for last 5 months. Now since yesterday it has been reduced to 5 mg, my col levels are good with diet exerciser and
total colestrol-116
Triglicerides- 110
HDL- 37
Non HDL colestrol 79
LDL- 57
IS Statins necessary for me if I can keep the cholesterol down by food and lifestyle.
Could Statins be the cause of the wt loss.
thanks
Bhuvanesh Sharda
Hi Bhuvanesh,
I’m unable to give you that kind of advice. Only your doctor who is most familiar with your entire medical history can tell you whether or not the statins are necessary. Perhaps you can discuss a switch to a different med if there is a reasonable substitute (?).
Kind regards,
Bill
Dr. Bill – This article and comments have been very helpful. I hope I am not duplicating something already covered …
Had a stent placed in the “widow maker” artery about 2 weeks ago. Doctor says the blockage was about 90%, and toward the bottom of the heart (not over it.)
Started to walk daily again, 3 days after procedure, and quit due to jaw pain – which I had had during exertion, and which alerted me to the need for the stent. Took 4 days off, and am now walking again. (20 minutes, very slowly.) Still having jaw pain, but not as intense as before the stent. It does abate when I return home to rest.
Do you think this will subside? I am also not sure if anxiety is contributing to this condition? Thoughts? Comments? Wisdom? A small part of me is afraid to walk, but I don’t want to end up totally inactive. Doctor is aware. Thinking I may need nitrate meds. Thanks.
Hi Greg,
Thanks for taking the time to leave a comment. I can certainly appreciate your concern. You mentioned that it occurred three days post-op, so bear in mind that it’s still early days and your heart is still in recovery mode. After all, you’ve just had a foreign object (catheter, balloon, stent) poking around the insides of your heart and this can create a bit of irritability until things settle down. If your cardiologist can confirm that there are no other sinister blockages that could plausibly explain this, then it may very well be just a temporary and transient passing discomfort.
While I obviously can’t give you any specific medical guidance, if you’ve been to your doc and and made him/her aware of the situation, then you’ve done the right thing. I’d say that if after a couple weeks this is still happening, then you might want to ask your doc for further work-up to see if something is going on further downstream from the widow maker (left main artery).
Regarding anxiety, congratulations, you’re normal. After something like this happens, it’s normal to experience a bit of anxiety and this could plausibly contribute to some physical discomfort. But if it persists, then you might also consider talking to a hospital social worker who is trained in helping people work through the mental aspects of going through a medical issue. I like to say that reaching out for help is a sign of strength, not weakness. We’re only human, and sometimes we need a little support.
Hope this helps.
Kind regards,
Bill
Hi Dr. Bill Sukala
I live in Italy. I amjust shy if 63 yr old female.
On my 60th bday I was cycling with my husband on our tandem when I experienced chest, jaw, back, arm pressure, burning, fatigue…Next day still not well taken to ER, then by Ambulance to a larger hospital in Piacenza, Italy. My parents both died of heart problems, so although I look fit, the signs were concerning. My cardiac enzymes normal, EKG normal, Stress Ultrasound with dye normal. Cardiologist said something is wrong, put me in for an angiogram. Right vent normal, left descending artery not so good (widow maker had 75-95+ blockage), and another blockage in a peripheral artery. Two stents with medication. Done.
I never really felt better after the procedure, certainly didn’t feel myself anymore. But about 9 months later started to feel better and better.
Then after a year was taken off one if the heavy duty meds that is like rat poison (Brillique sp). A few months later experienced a MINOCA. Thankfully no heart damage but cardiac enzyme troponin was elevated. Experienced funny pains, so was out back on the blood thinner, Brillique, and another med was added to the medication cocktail of BP, a Statin, cardiac aspirin, antidepressant (which I had been on for over 18 yrs, depression runs in my family), now a Beta Blocker added due to the MINOCA.
Then during all this also taking a med for GERD. And I had been experiencing what felt like angina, but at all time of the day or night. Finally a Cardiologist referred me to a cardiac hospital, they did a TAC CAT, and said that my smaller arteries had the micro spasms, and didn’t seemed concerned.
Then went back to the Cardiologist at local hospital, did stress test, EKG, bloods, etc, all normal, but this Cardiologist put me on Renexa for Angina, starting with 375, the 350 mg. I didn’t feel well, but she said it couldn’t be the meds. Three weeks later I was continuing to feel like a truck ran over me and had to go to the ER. The ER Cardiologist took me off Renexa and put me in a Nitro patch, 5mg for 22 he day time only. Still very tired.
Went to see my GP, he said to go off the nitro. He lowered my Statins, moved my BP med to the evening, and lowered the beta blockers.
I am finally feeling more normal again.
I still have GERD, and will get a check up for Helio Paloric Bacteria (sp?), And more bloods.
So far all my bloods, my end, my BP have been normal since my initial angioplasty.
My BP on meds is 110-120/60-80 depending on time if day ..
Pulse 58+
I’ve not had another angiogram for two years.
MY QUESTIONS—
I like to cycle on the tandem, as long as I feel ok, is this ok? We usually go 40-80 k/ ride.
Second Q, I am wondering if I can do any resistance training, like with their bands, or yoga? I was told not to do any isometric exercises. It’s all very confusing.
I’d like so swim, is this ok?
Lastly,when should I have another check up to make sure my stents are ok and not blocked? If I can avoid behaving an angiogram that would be preferable.
PS, All if these procedures…have taken place in Milan, Piacenza, and Pavia, Italy. Excellent medical care. But I’ve not been given any cardiac rehabilitation. I don’t think they offer this unless you are really bad. It would have been helpful to have some psychological support, but in the end I found my own. Still, not very helpful. I think because I look so fit people don’t think you need any guidance. Untrue. It’s been a life changing experience that continues to unfold,cand all while trying to communicate in Italian. Not an easy journey.
I hope you can offer some wise words, suggestions…
Thank you
Hi Jill,
Sorry to hear you’ve had a rough time with getting things stabilised, but it sounds like it’s coming good now. You’ve done a good job at being a strong advocate for yourself and following up for further studies. When it comes to the heart, sometimes it’s better the devil you know than the one you don’t know.
In answer to your questions, the most important thing is that your cardiologist has deemed you medically stable. If your follow-up appointments have consistently shown that your stents are still open and you’ve had no other signs or symptoms, then this is a good sign that you can get back to your exercise. However, cardiac issues aside, 40-80km is still a pretty good distance to ride for anyone, so I’d recommend working up to it slowly and steadily over time. That’s just good prudent exercise advice in general, but if you’ve had heart issues, then it just allows your body to adapt and can help reduce stress on the heart via improved fitness.
Resistance training with bands or similar is unlikely going to put any massive demand on your body such that it would cause a huge spike in heart rate or blood pressure. The main issue with any sort of isometric exercise or other high intensity weight lifting is that it can jack up your blood pressure and place stress on your heart. If you have a reasonably good aerobic fitness base, then this will certainly help reduce overall stress on your body and you should be able to tolerate resistance training without any issues.
Swimming is a nice aerobic exercise that is low impact and can deliver some good cardiovascular health benefits. I’d definitely recommend including it into your routine if it’s something you enjoy.
As for when you should have checkups, the only person that should answer that is going to be your cardiologist who is most familiar with your full medical history. Your appointments will likely be closer together just after your cardiac event and intervention but, over time, once you’re deemed medically stable, then the time between follow-ups might stretch out to a year. Again, it really depends on the individual and the cardiologist’s philosophy of what constitutes a good follow-up schedule.
Hope this provides you with some direction.
Kind regards,
Bill
Very informative. Thank you.
I had 2 stents after a coronary event. EF 67. My age 66. Fairly active prior to event. Discharged from hospital with very little info. Follow up with Cardiologist aka PA stated do what you feel you can do. I asked about Cardiac rehab and was told if you need to see the strip during exercise then sign up. I started my own cardiac rehab. I am not alone with poor follow up care. 7 weeks post MI and walking 1 hour at brisk pace. I am on low does of ACE inhibitor and beta blocker. Resting heart rate 50 to 60. Peak HR 126 while exercising. I feel great. Hope I am not killing myself. Need for better follow up by medical professionals.
Hi Lynn,
Thanks for taking the time to leave a comment. The good news is that your EF is normal, so this means that your heart’s pumping ability should be ok. Sorry to hear that you had a rough time in the follow-up process. If you’re now seven weeks post MI and you’re currently walking an hour at a brisk pace, then you’re well and truly on the right track. I also see that you’re only taking a couple meds, so this is good. Heart rates all appear to be reasonable too. The fact that you’re feeling good and are not having any signs or symptoms after your stents are all good indicators that you’re on the right track.
Moving forward, I would recommend just keeping alert to any signs or symptoms (if any) that might pop up. If you feel anything in the future that doesn’t quite feel right, then just be sure to get checked out and make sure there are no changes in your condition.
Also, be sure to keep your cardiologist follow-up appointments, as this will give you some additional confidence knowing that everything is clinically stable (i.e., heart rate, blood pressure, blood work, etc).
Hope this helps.
Kind regards,
Bill
@Dr Bill Sukala,
I can’t thank you enough and this is extremely helpful. I continue to do brisk walks daily and currently doing 3 to 5 miles a day with short intervals of light jogging. My workout sessions are twice a day totaling to 3 to 5 miles.
I am using my Fitbit to monitor my workouts as well as listening to my body.
I appreciate you taking the time to respond. The anxiety post MI is real and having your input has helped. I have kept all my Doctor appointments and will continue too.
Sincerely Lynn
Hi Lynn, thanks for the feedback. I’m happy to hear you found everything helpful. When it comes to your ticker, knowledge is power. Keep up the great work 🙏
Hi Dr Bill. I’m an insulin dependent diabetic injecting twice daily with humalog 75/25 mix. I’ve had chest pain and pressure on and off for the past month so went to my local clinic where a balloon angioplasty was performed without stent insertion. The reason for this was that plaque had built in one of the 3 stents I already had implanted 16 years ago.. Its over 4 days since the procedure and its been OK except this evening I went for another walk. I found myself walking faster than usual. Not deliberately. I just seemed to float along until I turned to go home. Within a few minutes I could feel something resembling pressure but not pressure if you know what I mean.im OK now but am wondering did I walk too fast to begin with and could my reaction be normal. I thank you Dr Bill. Cheers Kevin
Hi Kevin,
It’s hard to say exactly what happened but remember that you’re still in the recovery phase of your angioplasty procedure and there is still healing happening on the inside. Once you’re about four (4) weeks post-op and you’ve been back to see your cardiologist (who will presumably give you the all-clear), you should find that these little quirky things that can sometimes happen in the early stages will tend to dissipate on their own.
If for any reason you’re finding that this pressure is continuing to be an issue and is not resolving on its own, then it’s a wise move to follow up with your medical management team and let them know so they can bring you in for further work-up.
Hope this helps.
Kind regards,
Bill
Dear Dr. Bill I had angioplasty more than a year ago. I am a housewife and do all my work by myself. I lifted heavy objects yesterday and in the afternoon started to feel very bad. Like my heartbeat raising start shiffering and a funny feeling in my left arm. Do you think I could have hurt myself in the process of lifting some heavy furniture?
Hi Suzette,
It’s hard to say exactly what’s going on but it’s possible that you could have strained yourself due to the heavy lifting. If it’s something that persists, then it would be in your best interest to reach out to your medical management team (cardiologist, cardiac nurse etc) and run it by them to see what they think.
In general, if it’s a musculoskeletal issue, it should resolve on it’s own with rest. But sometimes, if it’s heart-related, it may persist even with rest or changing your position/posture.
Hope this is helpful.
Kind regards,
Bill
Dr. Bill, 10 days ago I had a stent place in my LAD which was 99% blocked. I did not have a heart attack, and no damage to my heart. I visited my cardiologist yesterday (not the one that did the procedure) and was told everything looks good and that I had no restrictions on activities. I don’t work out per se, but have lots of activities around our ranch. This morning, I raked leaves for about an hour. That pretty much wiped me out and I had pain in both shoulders and some in my neck. I have experienced this same pain, to a lesser degree since the procedure. I mentioned this to the cardiologist and she wasn’t concerned. Hoping to get your opinion.
Hi Dave,
Remember that after your angioplasty/stent that your heart is still in recovery mode, especially this fresh out of the procedure. It’s hard to say exactly what’s causing your discomfort but, as a general rule, you’ll want to minimise any heavier exertion for up to a month post-op. While it’s not open heart surgery, it is still a surgical procedure nonetheless and you will need some down time for your heart to settle down after being poked and prodded by the catheter and stent placement. Even if you’re feeling well (which is a good thing), this can fool you into overdoing it while your body is trying to recover. Most importantly, if your cardiologist is aware of this and isn’t overly concerned, then you are likely ok.
Hope this helps.
Kind regards,
Bill
Thanks for information+guidance one week ago left coronary with 90%stenosis in mid Lad.please can you guide exercises no other health problems. Thanks
Thanks. I’m glad you found it helpful.
Hello
Found this a very informative article, thanks for taking the time to write it and for sharing your expertise.
Much appreciated
Patrick
Hi Patrick,
Thanks for taking the time to leave a comment. Most appreciated 🙂
Just discovered your site while doing research on appropriate cardiac rehab. FYI, 78 years old, 10 years of cycling 4000 miles per year + resistance weights, ended up with 100% block LV, now stented and doing well. Did 18 mile ride @ 16 mph with HR in trying zone of 124 bpm the day before. Goal is to return to an appropriate level of activity ASAP.
In 10 minutes perusing your site, I’ve seen more relevant topics to my situation than I’ve managed to extract from my Interventional Cardio & Cardio Electrophysiologist.
Thank you for the superb work.
Cheers
Rick
Dear Dr Sukala, Thank you for this interesting article. I came across it as I recently had an angiogram – no further treatment needed as the blood flow was 97% – but have had chest pain when trying to run again afterwards. Is this to be expected? The angiogram was less than a week ago and I was over half-way through a 16 week marathon training program when I had to have the angiogram (i.e. running 4 times a week, including intervals and a long 14+ mile run). Thank you for any insight as to why I have seemingly just lost my fitness. Elisabeth
Hi Elisabeth,
Thanks for taking the time to leave a comment. While every case is different, it’s not unheard of to have some pain or discomfort after an angiogram given that it’s still an invasive procedure where they’re invasively poking around your heart with a catheter. Bearing in mind, the angiogram was, as you said, less than a week ago so it’s still early days and there could be some residual irritability from this.
I would recommend speaking to your cardiologist as a precaution and to rule out any cardiac source of the pain. Is it possible the discomfort could be coming from something musculoskeletal given that you had a pretty high training volume? In other words, it’s plausible that the pain could be happening in tandem with the angiogram rather than being caused directly BY the angiogram. Ultimately, my words are only speculation and you should discuss this with your interventional cardiologist (or associated practice nurse).
For maximum peace of mind, it’s good to know that your blood flow is 97%. Most cardiologists I’ve worked with have a 70% blockage threshold where they’ll consider angioplasty and stent at that point. So in your case, it would constitute a surgical risk with no real clinical net value.
Hope this helps.
Kind regards,
Bill
Want to know the exercises after angioplasty and stent in carotid arteries
Please read the article first and I think your questions will be answered there.
Kind regards
I read your information on taking it slow with healing, recovery after stent. So I had a 90% and 70% blockage with 2 stents on Friday. On Sunday I wanted to see if I felt any difference when walking. So I walked up and down the street a few times but my street has a hill. So I went up and down it a few times slowly.
I felt something in my chest not real pain but just like I could feel the stents not happy with what I was doing.
So how can you tell if the stent does collapse?
I am taking your advise now and waiting several weeks to start walking again.
Thank you.
Hi Mike,
If you’re concerned, I’d suggest calling your cardiologist’s office and at least speak to the practice nurse. More than likely the stents didn’t collapse, but it’s not uncommon to feel a little twinge if you’re pushing your exercise intensity during the recovery phase. In general, I’d say to make sure that you keep your exercise intensity quite middle-of-the-range until at least a month post-angioplasty. Remember that even if you’re feeling well, there IS still healing happening on the inside and it takes a while for things to settle down after the interventional cardiologist was in there poking and prodding within your arteries. Hope this helps. Cheers, Bill
Dear Dr Bill, firstly what an uplifting and interesting article to read. My 61 year old husband had a drug eluting stent fitted 2 weeks ago in the LAD for a severe restriction- he didn’t have a heart attack just mild tightening of the chest, some breathlessness and discolouration in his face – he had just finished a 2.5k open water swim. His troponin level was 18 and he did have fluid on his lungs(so there was a query as to whether it was SIPE or coronary or a combination of both)
Resting heart rate was and still is around 48. His ejection fraction measurement is 61, he was told this is excellent. Like many who have commented before he is desperate to get back to ‘ normal’ exercise for him which is 3-4km swim in open water/day.
We have asked for a treadmill assessment but they don’t do them in our area, our question is how soon does he wait before resuming normal training.
With many thanks
Belinda H (UK)
Hi Belinda,
Thanks for taking the time to leave a comment. The good news is that your husband did not have a heart attack and, given his ejection fraction is still quite good, it would appear he just had the plumbing problem in the pipes rather than any damage to the walls of his heart. Also, quite importantly, the fact that he got help in a timely manner most likely contributed to his excellent prognosis.
While I cannot offer any specific advice, in general, assuming that he’s had about a month or so of recovery, is walking at a moderate pace with no discomfort, and has clearance from his cardiologist, he should be able to get back to his routine. It’s important to remember that now that his “volcano has erupted,” it’s a case of better the devil you know than the one you don’t know. At least now he is aware of what’s going on and is currently being managed by his cardiologist. I’m more concerned about the person who has all the risk factors and doesn’t yet know it.
Once he’s cleared to exercise, I would simply suggest that he ease back into it slowly and gauge how he feels during and after his training. If it feels ok, then he can gradually increase duration and intensity over time. It’s all about being as prudent as possible and not trying to straight back into “hero mode” on day one.
Hope this helps.
Kind regards,
Bill
Hi dr Bill! A great discussion about exercising after a stent, thank you.
I had a stent to open up the LAD, 90% blockage in late Feb. I’ve been doing cardiac rehab since, when the local authority can arrange it (London uk)- I cycle a lot for work but have avoided all the hills , and have a six year old, exercise itself! I’m 48 and slim – like your other responders not an obvious cardiac patient.
Recovery after the stent took ages however- I was very tired for months. Since the second round of cardiac rehab (two sessions a week in the gym- mainly tread mill and cross trainer) I’ve felt so much better but three days ago I went and moved big boxes of books to a charity shop- since then I’ve had more aches in chest (central and right) and right shoulder/back pain (could be my muscles as did have pain from luggging bike up steps too a while back)- might also be angst about arranging a big family holiday soon (so much to do!) but have taken GNT spray for first times ever since stent- not sure if made any difference though.
Could moving the boxes of books (about 75m x 4 boxes medium size full of Mary Berry to Oxfam) have done real damage to my stent/heart? Just as I thought I was getting better!
Helen
Hi Helen,
It’s possible that heavy lifting “could” cause issues with your stent, but more often this is the case in the recovery stages where the stent isn’t fully settled yet. If it’s been a while and you’ve been cleared for exercise by your doctor, the issue might be more musculoskeletal. Also, if you can change positions and the pain goes away and then comes back in other positions, then that could suggest musculoskeletal origin. Not a perfect science but just a little field test that we used in cardiac rehab. However, ultimately it is still very important to discuss these issues with your doctor just as an added caution. Hope this helps. Kind regards, Bill
Hi Doctor, I am 39 n got major heart attack on 8 oct 2022 n got a stented next day around 30 hrs later in LAD. Also got tissue damage as confirmed in echo. My EF is 30-35 % . Have no blockage in any other artery. Echo showed a LV apical clot 0.8*2.2 cm. So doctor prescribed additional blood thinners. My PT INR is 2.3 as desired by doctor. I want to know whether clot can dissolve with medication itself. And i am afraid if the clot can mobilize if i do some jumping while exercising. As i m doing 1 hr of aerobics n brisk walking daily. Its been 80 days to my stenting.
Hi Rahul,
A left ventricular apical thrombus (clot) after a heart attack can occur within 24 hours so you are very fortunate that they found this. Your doctors should be closely monitoring the situation and treating it with anti-thrombotic therapy to ensure it dissolves and does not pose ongoing risk to you.
The other thing to consider is your ejection fraction (EF%). It was 30-35% at the time of your last echo. Work closely with your doctor to monitor this over time to determine if the EF recovers a bit. There is a thing called “stunned myocardium” which can recover after a heart attack and regain its contractile properties again. Hopefully this will improve and help you feel a bit better when exercising or exerting yourself. Hope this helps. Kind regards
My doctor said I had a 85% blockage I exerciser.5 time a week I’ve been taking baby aspirin for over 10 years on blood pressure medicine. Blood pressure is under control. I work out five times a week no chest pains. Do I still need to have the stent
Hi Marjorie,
I couldn’t tell you what to do in this case because only your doctor is fully aware and informed of what’s going on inside your heart. But as a general rule, once you get to 70% or above, you’re getting into the danger zone where, even if you’re not symptomatic right now, if a plaque rupture occurs, it could mean a sudden heart attack. I’m not trying to scare you but this is a plausible possibility. I’m hopeful that you’ll work with your doctor to make the best decision for your overall health.
Kind regards,
Bill
Good day, Dr. Bill Sukala. I am an orthopaedic surgeon in practise. I had no interest in working out. I experienced a heart problem in 2021. For the same, cardiac stenting was performed.(Two- LAD and RCA). After a year since my stenting, I began exercising after receiving the all-clear from my cardiologist. I began with very little weight training(1-2kg) and light cardio. I stayed in touch with my cardiologist and kept up my usual exercise. i noticed that i am now comfortable doing exercise for an hour or so using a combination of aerobics, weight training and modest callisthenics. I workout while keeping a close eye on my general health and don’t let my body become exhausted.
You have given some truly good information. Please continue your fantastic work.
Finally, I can state that because each body is unique, it is important to recognise its demands and to move in accordance with them. Never overwork yourself. Keep yourself fit and healthy.
Hi Shailender,
Thanks for your comment! You’ve done everything in the right order and now you’re reaping the benefits. I find that when people push it too hard during recovery is when things can potentially go bad. It’s important to know that even if feeling better, there is still healing happening on the inside. Congratulations on your speedy recovery and feeling great!
Your article was extremely interesting, and answered many of the questions that I had, as I am a six-time, national tennis champ on the senior tour. I play competitive tennis. 3-4 X a week and had a stent put into my LAD I did not have a heart attack just slight pain in the center of my chest twice in one month for which I attributed to a pulled muscle that must’ve of occurred while serving or playing tennis. So for me to be a couch potato for a week and not do any house work was unbearable. Not to mention no tennis for a month.Ughhhh. I am on clopidogrel +325 MG Ecotrin. My stent was put in on April 7 of this year and I cannot wait to get back to swinging my racquet. I absolutely truly enjoyed your article. Any feedback you can give me would be greatly appreciated. Thanks again.
Hi Sandie,
I can certainly empathise with your situation. Being an active person makes recovery just that much harder. If you’re used to being active and then all of a sudden you can’t maintain that level of activity, it can be psychologically difficult.
In your case, the good news is that you had a plumbing problem more so than a “heart problem.” No heart attack means that all your cardiac muscle is still intact. It’s also a very good thing that you were smart in respecting the symptoms and going and getting checked out. A lot of people ignore these types of slight aches and pains and then it can mount into something major.
Overall, it sounds like you’re on the right track. I would only recommend to work closely with your doctor to find the balance between the meds and your quality of life. You didn’t mention anything about a beta-blocker, but these are commonly prescribed with a stent and can make you feel slow and sluggish. So if you notice any side effects from the meds, I’d say to discuss with your doctor and perhaps work on lowering the dose over time, so long as it’s safe and prudent to do so.
Good luck!
Hi,
My father is 65 and just had a massive heart attack. He got two stents put and is in recovery in the ICU. The doctors on the second day tried to put him in a chair to sit down but his pulse increased to 150bpm. He is on oxygen as well. I wanted to know if that is alright ? I’m scared for him. Also would like to know when is a good time for him to leave hospital.
Pls help. I need to have a plan for him. The doctors in my country scare me.
Also, what questions should I be asking the doc??
Pls help..I’m desperate.please
Hi Shiv,
I’m sorry to hear about your father. I can imagine that’s extremely stressful for you right now.
Ask about the ejection fraction percentage (EF%). This will give you an idea of how much damage there was to his heart muscle. Anything 55% or higher is good, but the lower it goes, it means there was more damage and it may affect how effective his heart is able to pump blood in the future. So ask the doctors about this and also what the likelihood is of his heart recovering some of its contractile properties over time as he recovers from his heart attack.
You’ll also need to know what medications they’re going to put him on and the effects of those medications. More than likely they will put him on beta blockers which will slow down his heart rate, probably an anti-platelet medication like clopidogrel, maybe a low dose of aspirin, and a statin. You’ll need to know how these will affect him in general, but also if he is going to do any form of exercise or physical activity. Medications can affect his ability to do activities, such as beta blockers which can significantly slow down his heart rate and affect his exercise capacity and tolerance.
You’ll need to ask the doctors about the recovery process. How long will it take for him to leave the hospital? What is the full recovery time? What are the limitations on what he can and cannot do while he’s recovering? Is there a cardiac rehabilitation program that he can attend in order to get extra attention while he’s recovering.
He will likely be able to leave the hospital once the doctors deem him to be medically stable. If he just had a heart attack and stents, he may be in the hospital for several days or longer, depending on how much damage there was to his heart muscle.
I hope this helps point you in the right direction.
Kind regards, Bill
Dear Doctor Sukala
Most interesting information. One question however:
some five years ago I had chemotherapy for metastatic cancer. I am now in remission and Aberaterone + zoladex has just been changed enzalutamide + zoldex three weeks after being discharged from cardiac unit where I had one stent inserted by which time my muscles had perished although I persevered and completed rehabilitation course, I find that my muscles and joints ache which do not motivate me to do any exercises.
Any suggestions on how I can get back to exercising. Are used to do Pilates and yoga for 10 years prior. It seemed to stream muscles and him joint pain each time I return to exercising.
Could you please advise on how I can commence exercising.
Many thanks.
LES
Hi Les,
Sorry to hear you’re having a difficult time with everything. Remember that it’s still early days after having your stent placed and there is still some healing happening on the inside. Regarding your muscle and joints aching, it is possible this could be a side effect of the medications so I would suggest that you discuss this matter with your doctor to see if it’s the medication causing it and, if so, are there any other medications you could try which might still serve their purpose but without the side effects? Did this joint and muscle pain ONLY start after you started on the new medications? Once that’s sorted, then it will be important to ease back into your exercise and build up your tolerance slowly. You might also want to find a Pilates studio that has staff that are qualified to work with people with medical issues. That way they can ensure that you’re progressing safely.
Hope this helps move you in the right direction.
Kind regards
Bill
Hello, Dr. Bill!
Hope you’re still active here; I just discovered this valuable site.
My brief story: 75 yrs old, lifelong fitness buff. 2 hour workout every other day (lifting & cardio), hiker and climber, “exceptional” treadmill stress test results earlier in the year, etc etc.
Recent labs including lipid profile were good, though in previous years I’ve tended toward high triglycerides, low HDL, highish LDL. No symptoms ever, until BAM.
99% proximal LAD “hazy” blockage, troponins peaking at about 3400. Ejection fraction dropped from mid 60s to 50-55. Got an angio/eluting stent and here I am. Just had my 2-month anniversary. On Prasugrel 10 mg and Atorvastatin 40.
So now I’m back at the gym 3 days a week, cardio plus lifting. My cardiologist, who’s known me for 20 years, felt I was beyond typical cardiac rehab. Not pushing heavy weight, I’ve ramped up to maybe 60-70% of what I was doing some months ago. Cardio, I hit my target HR on the elliptical and go for 25 minutes, with what I’d call moderate intensity.
But my progress is a little slower than I’d hoped. I can still feel the occasional slight breathlessness, the now-and-then weakish feeling in the knees. These almost feel like anxiety symptoms, but who knows. Like everybody else in this boat, I’m now hyper aware of all things cardiac.
My question: can I regain that EF? I’m thinking of expanding my cardio to 5 days per week, just to force the recovery trend a little more. I’ve been looking for papers on rehab protocols for older athletes – OK, “very old” as the literature so charmingly puts it – and there’s almost nothing out there.
Anyway, any input is most appreciated. Wish I’d discovered this resource sooner!
Hi Dr Sukala, thank you for the informative article. I have a weird situation. Had an emergency stent placed in my RCA on Feb 14th, yes got a real heart gift! Started with Brilinta and aspirin. Switched to Plavix after a week as I became severely allergic to Brilinta. Continued having on and off chest pains, was given nitro (under the tongue). Then they added Isosorbide Mononitrate 30 mg but within 4/5 days I had extreme adverse reactions, so they stopped. Next week started Metopropol Tartrate 25 mg and in less than a week had extreme reactions to it with bp crashing to 80/52, etc. Next week they tried Isosorbide Dinitrate 5 mg (with 1/2 tab for 2 days and then full tablet). By the end of the week the reactions started again with bp crashing, etc.
Finally my cardiologist declared I’m a person with a unique and ultra sensitive system, so a minimum of meds. Strongly advised me to stop as soon as the chest pains start and if it gets worse start with an acetamenophen and then proceed to the under the tongue nitro.
I then started cardiac rehab. Have completed 4 weeks, but its very, very, very slow because my heart rate keeps going up and they have to stop me. Now I’ve noticed my ankles swell up if I’m up and about too long. Have to frequently take breaks with my feet up. Have been able to manage the chest pains with Tylenol and resting.
But, I feel I’m half or even less the person I was!!! I can barely do anything, thankfully I’m retired, but I’m so frustrated and not sure what’s going on.
Can you please, please give some insight? All my research shows that after stenting people can back to almost normal lives with some lifestyle changes. We already ate healthy, but I’ve further reduced salt and portion size. But I’m not losing weight. I feel I’m turning into a vegetable! Please help. Will appreciate any insight or recommendation and I promise you I won’t hold it against you. At least it will give a point/direction to ask questions or try something different. Please help. Thank you. Joy
Hi Joy,
Thanks for sharing your story. Wow, you’ve been through the wars with all this going on. As you said, in most cases, people return to normal pretty quickly after a stent, but there are always those rare exceptions.
Based on the information you’ve provided, it’s interesting that you had the stent in the RCA and yet you’re still experiencing chest pain. I would be pushing the doctors to do more investigation into why you’re having ongoing chest pain. Are they absolutely certain that there are no other obstructions in any other arteries?
Did they give you any information on your cardiac enzymes such as troponin? What about your ejection fraction? These numbers can give an indication as to whether or not there was any cardiac damage. Hopefully not. If it’s only a plumbing problem (meaning the arteries), then that’s better than having heart muscle damage.
With regards to the cardiac rehab, has the rehab team noted that your heart rate is going up anomalously high, more than what they would consider normal? If so, this might also be something worth investigating. Also, is your heart rate predictable at a given workload. If you are doing 3.5 mph on the treadmill and your heart rate goes to 120 bpm, and then you do 3.5 mph on a different occasion, does your heart rate also go to 120 bpm again? Is it consistent or is it all over the place?
You also mentioned your ankles are swelling up. Are they swelling up with fluid? I’m just surprised that this has not been flagged and dealt with.
As for your diet, it sounds like you’re conscientious and aware of what you’re putting into your mouth. With regards to your body weight, remember that if you’re retaining fluid (something to do with the swelling ankles), then maybe that could be a factor in your difficulty with losing weight which has nothing to do with body fat.
So in summary, I’d be talking to your cardiologist about the following:
1. Ongoing chest pain. If you had the angioplasty/stent and your artery is open, then what is provoking the pain you’re having now?
2. Was there any cardiac muscle damage? Ask about cardiac enzyme tests and your current ejection fraction.
3. Why is your heart rate acting erratically in cardiac rehab
4. Why are you having edema (swelling in your ankles)?
I wish I could be of further help but, if I was in your shoes, these would be my questions based on the info you’ve provided. Feel free to stop back and leave another comment because this can help other readers who may find themselves in a similar situation.
Kind regards
Bill
Hi Dr! So my background is 55yo male, 4 stents installed (emergency) Feb of 2023.
Meds: Brilintin, Arvostat,Lisinoprol,Metprolol no nitrates. I take 100 mg Viagra recreationally for ED.
I train cardio and train hard during the hottest part of the day here on the East Coast, direct sunlight, on a turf football field. Been doing this pre heart attacks, and picked up 3 weeks after i got released in 2023. I want to stress, i really really push myself, and the elements. Been an athlete and still train as such. I feel so so so good after I’m done, with that combo of heat/humidity/sweat.
My questions are, i do this 8-9 days in a row take a day off then repeat. from April until October, then I’m inside of a gym. I usually just do a spinning class for a hour, do some light weights and thats it. Why is it after a year and a half, my warm up’s and first 2-3 sprints (100 yds) i am completely 100% gassed? I mean i am huffin and puffin, for lack of better words…then the 4,5th sprint, its like the door opens, and i can literally sprint, full speed, and not get tired or out of breath. But when I’m done and I’m cooling off, maybe walking a lap, or 2 and try to sprint again, I’m toast at that point, and thats when i quit for the day. My blood pressure is back to 115-ish /over 60-ish after workouts and will remain that way. My particular cardiologist tells me to do what i can handle…would love to hear a different opinion from you!! Im so glad i found your website!!
George
Hi George,
Thank you so much for sharing your story and background—it’s clear you’re incredibly dedicated to your fitness and passionate about staying active, which is commendable, especially after your health scare in 2023. Your commitment to training hard and pushing yourself in challenging environments is inspiring.
What you’re describing with the early fatigue followed by a breakthrough after a few sprints is actually quite common and can be influenced by several factors:
Medications: Some of the medications you’re taking, particularly Metoprolol (a beta-blocker), can blunt your heart rate response and make your body slower to adapt to the initial demands of exercise. This might explain why the first few sprints feel so tough until your cardiovascular system “catches up.”
Progressive Warm-Ups: Given this, you might benefit from a more gradual warm-up routine. For instance, start with 5–10 minutes of light jogging or dynamic movements to ease your body into higher-intensity work. This can help minimize that initial “gassed” feeling.
Training in the heat and humidity adds a significant layer of stress on your cardiovascular system. While it’s great to challenge yourself, ensure you’re staying hydrated and replenishing electrolytes. Dehydration can make your workouts feel harder and affect your recovery.
Your training schedule of 8–9 days in a row with just one day off is intense. While you may feel good overall, even the fittest bodies need recovery time to repair and adapt to the stress of exercise, particularly in extreme conditions. Consider incorporating more rest or active recovery days (e.g., light walks, yoga, or swimming). This could help with the “toast” feeling you experience when you try to sprint again after cooling down.
You mentioned using Viagra recreationally for ED. While it’s generally safe for most, it can sometimes impact blood pressure regulation during exercise, especially in combination with your prescribed medications. This is worth discussing with your cardiologist to ensure there are no interactions affecting your performance or recovery.
That amazing post-workout feeling is likely the result of endorphins, improved circulation, and a sense of accomplishment. It’s a great motivator, but just make sure your training intensity and schedule are sustainable for the long term.
Your cardiologist is right in advising you to do what you can handle, and it sounds like you’re listening to your body and adjusting as needed. Keep in mind that recovery is just as important as training, especially as we get older. A few small tweaks—like longer warm-ups, more hydration, and a bit more recovery—could help you feel even better during your workouts and extend your ability to train hard for years to come.
If you have any other questions, feel free to ask. I’m glad you found my website, and I wish you all the best in your fitness journey!
Warm regards,
Dr. Bill
Hi Dr, my wife started rebounding for exercise due to her arthritis and she loves it. I had a stent in main artery, done next day after my first stress test in February, doing well. Is rebounding ok for me? I had no heart attack or heart damage. Great article thanks.
Hi Alfred, as long as you’re medically stable and cleared for exercise by your cardiologist, you should be ok. Once the stent is healed and settled, you should be ok to start rebounding. Cheers
I’m having a aortagram with a stent placed in my celiac artery due to compression from the outside by nerves and adhesions and median arcuate ligament release in Nov 2022 and open surgery 2023. I had an Angiogram angioplasty balloon in 2023 and had minimal blockage. Diagnosis is MALS.
Unfortunately the celiac compressed again requiring a stent soon. How long is recovery and when can I play competitive tennis and pickleball?
Thank You. Very informative informative.
Hi Barbara
Thank you for sharing your situation — it’s clear that you’ve been through a lot with your diagnosis of Median Arcuate Ligament Syndrome (MALS) and the subsequent interventions. Let me address your questions as thoughtfully as possible:
Recovery after stent placement
The recovery period after a stent placement in the celiac artery can vary widely depending on individual factors such as overall health, the extent of the procedure, and how your body heals. It’s important to follow your doctor’s specific instructions regarding activity levels in the weeks following the procedure. They will likely recommend avoiding strenuous activity during the initial recovery phase to allow proper healing and ensure the stent remains patent.
Returning to tennis and pickleball
Resuming high-intensity sports like tennis and pickleball should only be considered when your medical team gives the all-clear. These activities place significant demands on the cardiovascular system, so it’s essential to ensure that:
–The stent is functioning well and there are no complications.
–The surrounding tissues have healed adequately.
–Your cardiovascular system can handle the exertion without risk.
Your doctor might recommend gradually easing into physical activity and monitoring your symptoms closely. This could involve starting with light exercise and progressively increasing the intensity under medical supervision.
Follow-up and tests
It may also be worth discussing with your doctor the possibility of follow-up imaging or a treadmill stress test. These can provide valuable information about your heart rate, rhythm, and blood pressure response under high intensity exercise loads. This will better inform their recommendations to you.
Monitoring symptoms
Be mindful of any symptoms during activity, such as pain, fatigue, or difficulty breathing. These could indicate that you’re overexerting yourself or that further evaluation is needed.
Final thoughts
Ultimately, your medical team knows your specific case best, so their guidance should always take precedence. I encourage you to work closely with them to develop a safe and realistic plan for returning to the sports you enjoy.
Wishing you the best in your recovery and hope you’re back on the court soon when the time is right!
Warm regards,
Dr Bill
Thank you for a very straight forward explanation.
I’m itching to get back to my best and my procedure was 18th October 24
My cardiologist has advised me that in the future only moderate exercise is advisable.
he was very adamant about this..
This is hard to accept considering how fit and extreme my training was prior to the stent procedure.
He has suggested that even with 2 stents fitted I’m at high risk of a heart attack.
I have a resting heart rate of 58 Bpm and up until the plumbing incident I could get my heart rate at 195 bpm max,
My training consisted of Short sharp interval training and long endurance rides.
I would ride my bike for hours with an average HR of 140-160 BPM.
He did prescribe Beta blockers, but they made me lightheaded.
I did not have a heart attack, but he did say the arteries lower down, there was some blocking but he felt medications would sort those out
his initial report was
LMS: Patent
LAD: Critical proximal course lesion. disease in large calibre first diagonal branch (0,0,1)
Lcx: trivial plaque disease
RCA: trivial plaque disease
post report
Overlapping 3.0×12 and 3.5x38mm stents back to proximal LAD
Post-Dilation with 3.5/4.0/4.5mm NC Balloons:
IVUS confirmed no edge dissection and well expanded and apposed stents
good angiographic result
IMP: Successful provisional PCI to LAD/Diagonal using DCB and 2 Onyx DES:
Why would he recommend this corse of action and would you agree with him.
I do have a few other conditions, underachieve thyroid, CKD stage 3, prior to the event high blood pressure, (it’s very good post stents) high cholesterol
I have not drank alcohol for 20 years
ex smoker gave up 25 yrs ago
eat healthy 80% of time
Ride my bike 5-6000 miles per year
62 yrs of age
cardiologist says high risk factors Hypercholesterolemia, Hypertension, Former Tobacco Use
is he just being cautious?
your comments would be enlightening
Hi Paul,
Thank you for sharing your story and providing such detailed information about your background, procedure, and current health. It’s clear that staying active and maintaining your fitness has been an important part of your life, so I can understand why this shift to more moderate exercise feels challenging to accept. Let me address your main points step by step.
1. Your cardiologist’s recommendations
Your cardiologist’s advice to focus on moderate exercise is likely grounded in your specific risk factors and medical history. These include:
High-risk factors: Hypercholesterolaemia, a history of hypertension, former smoking, and CKD stage 3 all increase your cardiovascular risk.
Recent Procedure: While your stents have restored blood flow, the critical lesion in your LAD (widowmaker artery) and plaque disease in other arteries suggest that your coronary system is still vulnerable.
Preventing Overload: Intense training, like short sharp intervals or long rides with high heart rates, places significant strain on the heart. Your cardiologist may be advising caution to minimise the risk of overexertion leading to complications, such as a heart attack or further arterial damage.
2. Resting hr and fitness level
Your resting heart rate of 58 bpm and history of endurance training show you were in excellent cardiovascular shape before your procedure. However, the presence of coronary artery disease (CAD) changes the dynamics. Even a well-trained heart can be at risk when arterial blockages exist, and fitness alone does not eliminate the underlying atherosclerosis that led to your stent placement.
3. Beta blockers and exercise tolerance
Beta blockers are often prescribed after stent procedures to reduce heart rate and blood pressure, easing the workload on the heart. However, the lightheadedness you experienced is a common side effect, particularly in those with low resting heart rates. If you’re not currently on beta blockers, it’s important to discuss alternative options with your doctor to ensure your heart remains protected while maintaining your quality of life.
4. Understanding the intervention and post-stent risk
Your post-procedure report indicates a successful intervention with well-expanded stents and no edge dissection. However, the presence of residual plaque disease in other arteries and your high-risk profile justify a cautious approach. Stents address the immediate blockage but do not reverse the underlying disease. Managing these risks with lifestyle changes and medications is essential for long-term prevention.
5. Exercise and risk mitigation
Moderate exercise is highly beneficial for managing CAD, improving vascular health, and reducing overall cardiovascular risk. While it may feel like a step down from your previous routine, you can still enjoy cycling and other activities at a less intense level. Consider these strategies:
Structured Training: Aim for steady-state rides at moderate intensity, keeping your heart rate in a range that feels sustainable (e.g., conversational pace).
Interval Adjustments: Replace high-intensity sprints with less demanding intervals that allow for longer recovery periods.
Consultation: Ask your cardiologist about a formal cardiac rehabilitation programme or exercise stress test to better understand safe heart rate zones for your training.
6. Lifestyle and risk factors
You’ve made remarkable lifestyle changes over the years, including giving up alcohol and smoking, which are significant achievements. Your 80% healthy diet and active lifestyle are commendable, but with hypercholesterolaemia and a history of hypertension, further dietary tweaks (e.g., focusing on heart-healthy fats, fibre, and plant-based foods) may provide additional benefits.
7. Is the cardiologist being overcautious?
Yes, your cardiologist is being cautious, but his recommendations seem reasonable given your high-risk profile and CAD history. While your fitness levels and history of endurance training are impressive, they don’t eliminate the underlying risks associated with atherosclerosis and plaque instability. The goal is to balance your desire for an active lifestyle with the need to protect your heart from further complications.
Final thoughts
It’s fantastic to see how committed you are to your health and fitness. While this new approach may feel like a significant adjustment, it doesn’t mean you can’t enjoy cycling and staying active—just with a focus on moderation and long-term health. Consider working closely with your cardiologist to fine-tune your exercise plan and seek additional guidance from a cardiac rehab specialist or sports cardiologist if needed.
If you have more questions, don’t hesitate to reach out. Wishing you all the best on your health journey.
Warm regards,
Dr Bill
Please i want tamil translation
Google Translate may help
Thank you very much for this article Dr!
I had a heart attack (huge pressure in chest with shoulders and arms contracting) 5 weeks ago. I had an stent installed with a 70% blockage of my left artery. The cardiologist told me it is due to my high cholesterol level (LDL 66mg/dl). I thought I had a decent lifestyle, playing squash 1-2 times per week 1.5h, soccer once per week plus occasional cardio and weight training, watching what I eat and not smoking.
I have two questions:
1- Can I play squash (max heart rate on my last session two days ago was 175bpm)?
2- The 80mg Lipitor that was prescribed to me after the intervention gives me joint pains, can I stop taking it?
Thank you very much!
Hi Sorin,
Thank you for reaching out and for sharing your experience. First, let me commend you on your proactive approach to understanding your health and managing your recovery. It’s great that you’re paying close attention to how your body responds post-intervention. Let me address your questions point by point:
1. Playing squash
It’s wonderful to hear that you’re eager to get back to playing squash, but it’s important to approach this carefully. At just five weeks post-heart attack, your body is still healing internally, even if you’re feeling good externally. High-intensity activities like squash can place significant demands on your cardiovascular system, particularly at heart rates like the 175 bpm you mentioned.
I strongly recommend speaking with your doctor about undergoing a treadmill stress test to volitional fatigue. This test will provide valuable insights into your heart’s performance, rhythm, and blood pressure under high-intensity conditions. Your doctor can then offer personalised advice on whether squash is safe for you at this stage and help establish heart rate zones to guide your activity.
2. Stopping Lipitor (Atorvastatin)
I cannot advise you to stop taking your Lipitor (atorvastatin) medication. Only your doctor can authorise changes to your prescribed regimen. However, joint pain is a recognised side effect of statins, and it’s worth bringing this concern to your doctor’s attention. You might ask if it’s appropriate to:
–Lower the dose from 80 mg to a smaller dose.
Consider switching to a different cholesterol-lowering medication with a lower risk of side effects.
Explore whether the benefits of continuing the high-dose Lipitor outweigh the side effects in your specific case.
–Healing and recovery
As you’re just five weeks post-heart attack, it’s important to remember that the healing process is ongoing. Even if you’re feeling better, your body is still recovering from the stent placement and adapting to your new medications and lifestyle adjustments. This is why it’s essential to work closely with your doctor and healthcare team to ensure you’re progressing safely.
In the meantime, you might consider lower-intensity activities such as walking or light cycling to stay active while giving your heart time to strengthen. Your doctor or a cardiac rehabilitation specialist can help tailor a programme that supports your recovery and fitness goals.
Final thoughts
Your active lifestyle prior to the heart attack is a strong foundation, and with the right guidance and care, you can work towards returning to the activities you enjoy. Please do discuss your concerns about both squash and Lipitor with your doctor—they are best positioned to help you navigate this phase of your recovery.
Wishing you all the best on your journey back to health and fitness. Feel free to reach out if you have further questions!
Warm regards,
Dr Bill