The prospect of having an implantable cardioverter defibrillator (ICD) installed can be daunting news.
Nobody wants a slab of metal inserted into their chest, but once you educate yourself on ICDs and the conditions they treat, you will find that you can live a relatively normal life and do most things you did before having it installed – only with our the worry of an arrhythmia stopping you dead in your tracks.
Your heart beats in a controlled rhythmic manner in order to efficiently deliver blood—and the oxygen and nutrients it carries—to different parts of your body.
Any disturbance in the heart’s electrical conduction system (arrhythmia) may compromise its ability to pump blood.
While some heart rhythm abnormalities like atrial fibrillation can be managed with anti-arrhythmic medications, in other cases, comparably more dangerous ventricular arrhythmias (i.e., irregularities propagated in the lower chambers of the heart) may require you to be fitted with an implantable cardioverter defibrillator.
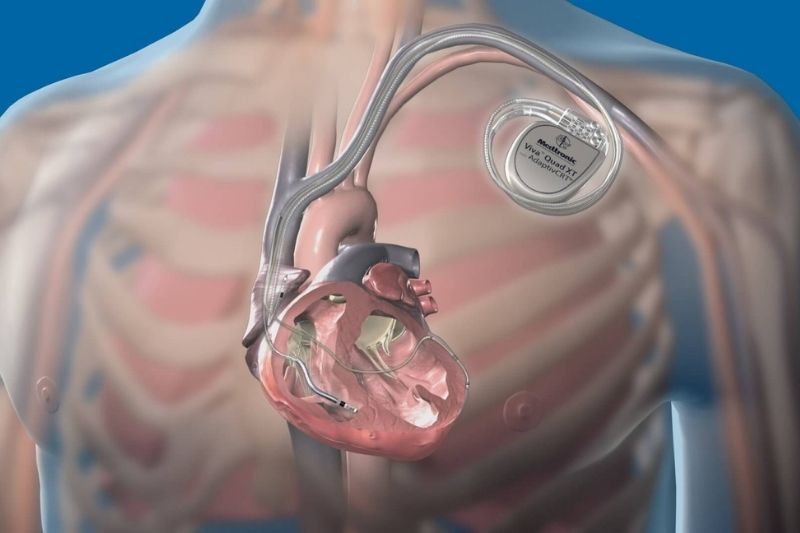
What is an implantable cardioverter defibrillator?
An implantable cardioverter defibrillator is a small, thin, battery-powered device implanted just under the skin in the chest region and is designed to deliver a shock to restore normal cardiac rhythm in those at risk for sudden cardiac death due to malignant arrhythmias like ventricular fibrillation or tachycardia.
These conduction disturbances may be the result of a heart attack, cardiomyopathy (diseased heart muscle), or a congenital defect, all of which can interrupt the normal electrical conduction pathways in the heart.
While the implantable cardioverter defibrillator may be an inconvenience at first, many of the ICD patients I’ve worked with in cardiac rehabilitation adjusted their lifestyles and went on to live quite enjoyable and productive lives.
Short implantable cardioverter defibrillator video
If you learn more easily by watching videos, here is a very short 3D animated clip about ICDs which explains the procedure in very simple terms.
Can I exercise safely with an implantable cardioverter defibrillator?
When I teach fitness professionals about training clients with heart problems, invariably the question arises, “how do I exercise someone with an implantable cardioverter defibrillator?”
My short answer is, not too differently from anyone else, except for several precautions (to be addressed below).
As a clinical exercise physiologist, I’m generally less worried about someone WITH an implantable cardioverter defibrillator because this tells me they’ve been diagnosed, treated, and are now under the care of a cardiologist.
It’s the person with malignant arrhythmias WITHOUT an ICD that keeps me awake at night!
As stated above, your implanted cardioverter defibrillator is designed to “zap” you back to normal rhythm in the event your heart starts racing or beating erratically.
Exercise also causes your heart rate to increase, but this is a normal and expected response.
So how does your implantable cardioverter defibrillator tell the difference between a potentially dangerous heart rate or rhythm versus normal exercise-induced increases in heart rate?
Generally speaking, your implantable cardioverter defibrillator will be programmed by your electrophysiologist to detect both abnormal heart rates and rhythms which are likely to be outside the range of what you’d accomplish with most daily activities or moderate exercise (which will minimise unnecessary or inappropriate shocks).
Your medical management team should give you safe exercise heart rate limits for your implantable cardioverter defibrillator settings.
Your doctor may wish to carry out an exercise stress test to simulate your usual exercise intensity and “troubleshoot” any problems before they happen.
Tips for safe exercise with an ICD
The following tips will help you safely return to (or begin) an exercise regimen, but please understand these are general recommendations and are not a substitute for your doctor’s advice.
- First and foremost, before you start or return to your exercise regimen, it is absolutely imperative that you are medically stable, your implantable cardioverter defibrillator has been fitted and programmed, you’ve been educated on your specific condition and understand your ICD limits, and you are well-managed (i.e., medications like beta-blockers which preclude your heart rate from climbing too high).
- Wear an ID bracelet and have your implantable cardioverter defibrillator card with you at all times. It will inform those around you of your condition if you are unable to speak for yourself.
- Exercise with a friend or family member who is familiar with your condition and knows what to do in the event of an emergency.
- The ICD can be affected by magnetic or electrical fields. In the gym setting, bioelectrical impedance analysis (BIA) is a technology used for assessing body composition (percent fat, muscle, water). You should avoid this and opt for something simpler such as the sum of skinfolds. Heart rate monitors are unlikely to cause any problems in the gym setting.
- If you’re an athlete with a congenital heart defect and are accustomed to training and competing at high intensities, you should discuss your specific situation with your medical management team. They can adjust your implantable cardioverter defibrillator settings to recognize the difference between a normal increase in heart rate from exercise and that associated with an abnormal heart rate or rhythm. Clearly an ICD is not the most convenient gadget for playing sports, but it will significantly minimize the risk of sudden cardiac death.
Exercise prescription for implantable cardioverter defibrillator
The four fundamental components of an exercise prescription are easily remembered by the FITT acronym: Frequency, Intensity, Time (duration), and Type of exercise.
So a basic exercise prescription for a person with an implanted cardioverter defibrillator might entail the following:
Frequency
No matter if you’re new to exercise or are already a regular exerciser, after your implantable cardioverter defibrillator placement (and perhaps recovery from a heart attack or other health concern) you may feel a bit tired and lethargic. If so, congratulations, you’re human and completely normal.
I suggest easing into exercise with a three-day per week regimen at first, and slowly add on days as your body adapts and you feel stronger.
In this case, I am referring to structured conscientious exercise with purpose. However, with regards to background activities,
I also encourage you to do daily incidental movement, such as walking to the corner shop for a liter of milk, down to the post office, etc.
There is a lot of new evidence surfacing in the medical literature which shows this background activity plays an important role in both weight loss and weight management.
Intensity
Intensity refers to how hard you’re exercising.
Once you get your ICD implanted, you should ease into your routine.
A sharp spike in heart rate could potentially set off your ICD.
Therefore, you should include a low-level 5 to 10 minute warm-up and cool-down phase for aerobic exercise (i.e., walking, cycling) to allow for a slow and steady increase in heart rate.
After that, work up to a low to moderate intensity.
A good pragmatic range is around 60 to 75% of your age-predicted max heart rate, but you can adjust this up or down depending on your relative fitness level and if it’s appropriate based on your physician’s advice.
In the exercise business, a best “guestimate” of your maximum heart rate is 220 minus your age. From this number, you then calculate a training heart rate range.
So if you’re 40 years old, then it’s 220 – 40 = 180 (theoretical max heart rate).
Next, 180 x 60% = 108 beats per minute and 180 x 75% = 135 beats per minute.
Therefore you would want to exercise in the range of 108 to 135 beats per minute.
If you have a hard time finding your pulse, get yourself a heart rate monitor or a Fitbit (which also tracks your non-exercise movement habits).
I have worked with numerous ICD patients who wore them and there is no concern of this interfering with the device. Check with your doctor if you have any questions.
The effects of beta-blocker medications
If you are taking beta-blocker medication, then your heart rate will remain blunted and will not fit neat and clean into the above heart rate calculation.
In this case, we like to use what is known as the Rating of Perceived Exertion (RPE).
There are two RPE scales out there, so to eliminate confusion, I will use the 0 to 10 scale.
In brief, 0 is sitting down at rest doing nothing and a 10 is an all-out effort to exhaustion.
Try to exercise at a “moderate” level, somewhere in the range of 4 to 6, and adjust based upon your body’s response.
Also take note of your heart rate when you’re at a moderate workload.
Though you may be on beta-blockers, this will reflect your individual response to exercise and can help serve as a guide.
If your dosage changes, then you may need to redo the above “experiment” to determine your new exercising heart rate.
In my professional experience, people on beta-blocker medications will see a heart rate increase of approximately 20 to maybe 50 beats above rest, but again, this is variable and will likely reflect the dosage.
Time (Duration)
The length of your individual exercise sessions will vary, but as with the other exercise prescription components, you may want to start off on the low end and progress to longer durations as your fitness levels improve.
For example, begin with a leisurely 15 to 20 minute stroll and see how your body responds.
Then work up to 30 minutes the following week, then 40 the week after, and so on.
Pay particular attention to the terrain.
Start off walking on level ground and, once your fitness foundation is established, you may want to experiment with some small hills (low incline).
Again, speak with your doctor regarding your exercise intensity and ICD limits.
This knowledge will help you to tailor your exercise prescription and reduce any fear or anxiety over getting shocked during exercise.
Type of Exercise
In this day and age, there are a million and one different exercises you can choose from, but the good news is that most fall into several broad categories.
The main types of exercise are aerobic, resistance training, and flexibility training.
For the purpose of this article, I will only discuss aerobic and resistance exercise.
Heavy duty power lifting or anaerobic interval training may not be conducive for individuals with an ICD (unless cleared by your doctor to do so).
Aerobic training
Walking, bicycling, ellipitical trainer, rowing machine, dancing, aerobics classes, etc are all popular forms of aerobic exercise.
Which is best?
The one that you enjoy most and are most likely to remain consistent with!
Resistance training (weight lifting) with an ICD
There are mixed reviews on whether or not resistance training (weight lifting) is appropriate for people with an implanted cardioverter defibrillator.
Much of this confusion stems from the belief that heavy loads will place large demands on the heart which will cause an arrhythmia.
While this is logical reasoning for very high intensity exercise, lifting lighter weights which do NOT leave you huffing and puffing and gasping for air are likely to be well-tolerated and can yield marked improvements in strength.
This, in turn, will make daily living easier, thus reducing the likelihood that basic activities will not set off your ICD.
To begin, start off with a weight you can lift in the range of 10 to 15 repetitions.
If new to weight lifting, begin with one set (i.e., one group of 10 to 15 repetitions) for the first couple of weeks and then graduate to two sets.
It certainly won’t turn you into a muscled bodybuilder, but it is sufficient stimulus to confer appreciable improvements in strength.
It is beyond the scope of this article to discuss every nuance of strength training, so I would suggest you hire a trainer for a few sessions to teach you proper form and technique.
Additional considerations for weight lifting exercise
- Avoid lifting weights so heavy that they leave you grunting, groaning, and gasping for air. This may increase the intrathoracic pressure, forcing your heart to work harder, and consequently set the stage for a possible arrhythmia (and subsequent shock). Rule of thumb: EXHALE ON THE EXERTION. In other words, when the weight is being lifted against gravity, exhale to release that internal pressure.
- Overhead lifting “may” put additional strain on your heart because it needs to pump blood “uphill” against gravity. You don’t necessarily need to avoid overhead movements, but may wish to use lower weights or do shoulder exercises like lateral raises or upright rows which minimize the overhead component. Bear in mind some overhead movements may aggravate the placement of your implantable cardioverter defibrillator, particularly if it was recently implanted. Stock standard advice: speak with your doctor for specific guidelines.
- Following on from above, in general, beware of exercises which might impact the physical placement of your implantable cardioverter defibrillator. For example, watch out for any exercises which incorporate the shoulder girdle/chest area where there is the risk of a weight or bar bumping into your implantable cardioverter defibrillator. If you’re doing flexibility exercises (i.e., yoga), be aware that certain movements could agitate the implantation site.
Prohibited exercises
- Contact sports or other activities which could result in a jarring effect to your body are not recommended or should be judiciously engaged in ONLY with approval by your medical management team.
- If you participate in water sports, you should do so with an exercise buddy in case you receive a shock, feel dizzy or lightheaded, or are disoriented and unable to exit the water by yourself. SCUBA diving is generally discouraged, perhaps due to the risk of drowning (if you are rendered unconscious). Then again, the best advice is to seek the advice of your medical management team who will be most familiar with your unique situation and best qualified to give you specific guidance.
Take home message
Appropriate exercise specific to ICD implantation can enhance your overall well-being and quality of life.
Regular training promotes healthy changes in the muscles and your collective cardiorespiratory (heart and lungs) system which, over time, makes your day to day living much easier.
Weight loss stemming from a healthy lifestyle reduces the overall load on the body and further reduces stress on your cardiovascular system.
As a result, your heart will not have to work as hard to meet metabolic demands, therefore reducing the load on the heart and consequently lessening the chances of an arrhythmia – and a shock from your implantable cardioverter defibrillator.
If your Interventional Cardiac Defibrillator (ICD) is one of the over half of unnecessary ICDs cited by Duke University, you can manually manage the defibrillator between its two modes of being a pacemaker and a surge device. Exercises that expand the chest will alert the pacemaker to bring down the heart beat. You will probably feel cold and the muscles will become constrained. Exercises that extend or press on the left arm will make the defibrillator surge and increase blood flow to the muscles. To get mobility and motion, practice getting out of the pacemaker mode and surging the defibrillator. The Boston Scientific rep explained to me that because of being thinner than most Americans, my muscles were more sensitive. The Boston Scientific rep helped close the sale of the ICD at Newport Beach’s Hoag Hospital, just one month after their FDA recall. PacificHospitalists.com has oversight of Hoag Hospital and collaborated with United Health Care (UHC) insurance to get paid for the ICD that was non-evidenced and out-of-guidelines. Over ten tests of heart, neurology, blood pressure and diabetes were normal. Five providers billed for 27 chest X-rays over two weeks despite no heart problem. One provider billed for 10 chest X-rays, apparently feeling ten was the threshold for being unnecessary and fraudulent.
The information on resistance training in the article was exactly what I was looking for. As a 17 year old with ARVD I have been left to discover my physical limitations on my own (my doctor is pretty hands-off when it comes to suggestions on exercise and my cardiac rehab program has limited knowledge of my condition and is more aerobic exercise focused). I have a good understanding of my aerobic abilities but did not know much about weight training. The suggestions in this article have a solid foundation of safety but also provide patients with a liberal guideline for exercise. Very encouraging to see a cardiologist with a balance between practicality, caution, and encouragement. Thanks!
Hi Sam,
Thanks for your comment. I should correct you that I am a doctorate-level exercise physiologist and not a cardiologist. While the information provided in my article should not supercede the recommendations of your doctor, it is at least a general guideline to put you in the right direction. In many cases, signs and symptoms must be monitored before, during, and after exercise. Err on the side of caution and gradually work up in both intensity and duration. The more information you know about your condition, the safer you will be. Please feel free to post another comment if you have further questions. Thanks for the kind words and best wishes to you.
Cheers
Bill
I like this article for the information but there is still one question I have been getting mixed answers about and I thought maybe someone could help.
I’m 28 and 2 years ago I was diagnosed with Brugada Syndrome. I asked my cardiologist about lifting weights and he told me I am completely healthy for doing such a workout however I need to stay away from push ups, pull ups, and bench press because of the led wire going between my clavicle and top rib. he said I could fracture the wire.
Then less than a year later another doctor told me is was nearly impossible to fracture the led wire because its so strong.
So long story short, is it possible to fracture the led wire by performing exercises such as push ups, pull ups, and bench press?
My Doctor no bench press I going to do it any ways I not going to loose my body if I die then so be it
@Michaelanthony,
Hi Michael, how are you? I got my ICD last week. Bench press is my most favorite exercise. Are you doing them? Are you still alive? Lol.
@Michaelanthony, I feel the same way. ICD, April, 2023. I was given the same restrictions but I was a bodybuilder and still an art figure model(nude) so it is full steam ahead to stay in top prime shape as a model. My Faustian Bargain.
Thank you for posting this information. After years of wondering what was going on, trips to the ER, and misdiagnoses, I was finally diagnosed correctly with CPVT (at 43 y/o!) last January. I have an ICD now and am on a betablocker. I was a recreational marathoner before this happened (yes, I’m lucky to still be alive), and I have found adding resistance training invaluable to my recovery. I have worked my way back up to a half-marathon and am training for a November marathon, however I am SO MUCH SLOWER (as in 3 minutes a mile slower) than I was before the ICD and beta blocker. I use PLE as my guide, and I don’t see any increase in my speed (or decrease in PLE) even with increased, focused training. Is this what you’ve seen?
Hi Ashley,
Sorry to hear you’re having a rough time with your training, but I am happy to see you’ve been correctly diagnosed and properly managed. Without working with you myself or being fully aware of your entire medical history, I could not reliably comment on your situation. I would advise you to find a university-qualified clinical exercise physiologist in your area who may be able to work with you and give you more specific guidance. Though you are right to note that beta blockers can sap your energy and leave you feeling lethargic. This might be something to discuss with your doctor regarding your dosage. Best wishes to you in your upcoming marathon!
I am 66 and I have undergone CABG in 1996 and angioplasty in 2004. In April 2012 ICD implantation was done due to VT.My cardiologist has advised not to lift left hand above the shoulder but I presume this restriction was for first 6 weeks. I have now started 45 minutes brisk walk daily and I found myself quite energetic after exercise. But before ICD implantation I was regularly jogging for 45 minutes. Can I start it again?
Hi there, and thanks for your comment. While I cannot legally give specific advice to any one individual (there are many factors and I am not familiar with your entire medical history), there is evidence that the benefits of exercise with an ICD far outweigh a sedentary lifestyle with an ICD (in terms of weight management and other cardiac/metabolic risk factors). It is great to see that you’re performing 45 minutes of brisk walking which, in the grand scheme of things, may not be too far off of a slow jogging pace. The most prudent course of action at this point would be to ask your cardiologist if there are any concerns about your picking up the pace a bit. Provided the ICD is stable and you’re not doing too much aggressive upper body (arm/shoulder movement), your doctor may give you the green light to go a little faster. Hope this helps!
Six months after successful afib ablation (and finding heart failure) and continued 10 miles/day biking, walking and swim exercises, i (70 yo) had an ICD implanted because my ejection fraction was still only 25-30%. Since the ICD implantation, I have experienced 8 inappropriate shocks while cycling due to SVT and the ICD’s inability to distinguish between SVT and VT or VF (including an electrical storm of 5 shocks) I’ve had no incidences of VT or VF. My doctor agrees with me that the ICD should be removed because my quality of life has led to PTSD. A recent second echocardiogram reading estimates my ejection fraction at 30-35% but my doctor thinks it’s more like 40-45% and I will have a MUGA procedure to get a more accurate EF. I will be getting a second opinion by a well known cardiac electrophysiologist who advises endurance athletes and has wriiten a book about the haywire heart (and exercise). Have you had patients with similar issues with ICDs, SVT while exercising and inappropriate shocks?
Hi Sandra,
Thank you very much for your comment. I’m sorry to hear you’ve had a rough time with your ICD. I’ve had a number of people I’ve worked with over the years that have had inappropriate shocks and, yes, it can be traumatic, especially when you’re trying to exercise.
Honestly, I would say you’re on the right track by consulting a cardiac electrophysiologist with experience helping athletes. It’s definitely a balancing act between getting the intervention right and not compromising your quality of life.
One of the things I would strongly suggest discussing with your doctor is your peripheral adaptations to exercise. I’ve worked with patients who were severely compromised in terms of their ejection fraction but due to their level of fitness, their exercising muscles (i.e., legs, arms etc) were extremely fit and efficient at extracting oxygen and nutrients from the blood. In other words, their fitness compensated for their reduced ejection fractions. One guy in particular had a very low EF but he was a highly trained cyclist that just kept on going and his heart didn’t really slow him down that much. The human body is pretty incredible when it comes to compensatory adaptations, so I wouldn’t hang your entire hat on just EF as a sole indicator of health and fitness.
In short, it sounds like you’re on the right path and I would suggesting discussing all of your concerns regarding exercise and quality of life with the new doctor to see about getting on a better trajectory.
Hope this helps.
Kind regards,
Bill
Thanks for this very good information. I found it very interesting.I have an Icd which has gone off twice with physical activity.I have now learned to watch it and I’m thinking about a heart rate monitor I see my electrophysiologist soon and I will discuss this with him.
Do you really want the negative in this sentence:
“This, in turn, will make daily living easier, thus reducing the likelihood that basic activities will not set off your ICD.”
Thanks for your Guidance. I had a defibrillator installed 5 weeks back (@ 43y/o).
I am looking for some prescription exercise within Canada for people with ICDs. Is swimming a good exercise after full recovery from ICD surgery.?
Hello Parag, thank you for your comment. Once you are fully healed up, I suggest speaking to your cardiologist to ensure that the swimming motion won’t disrupt the ICD wires. The other thing to consider is if it discharges while you’re swimming. May be best to employ the buddy method to ensure you have someone looking out for you. Provided your doctor gives you the all clear, then you should probably be able to get back to your swimming. Write another comment after you’ve fully recovered and let us know how you’re going. Best of luck.
National guidelines in many countries, as well as the scientific literature itself, continually advise professionals to avoid overhead resistance training “at first”. However, there is never a discussion about the time course for when it becomes safe or exactly what movements can be done once you’ve passed the “at first” threshold.
There is a serious need to educate allied health professionals on WHY it becomes safer after a period of time. Also, coordination between exercise physiologists, trainers, and cardiologists to determine specific weight and movement thresholds for pacemaker/ICD patients would make environments like CR that much safer and effective.
I couldn’t agree more. It is definitely one of those nebulous areas of exercise physiology/cardiac rehab. In the absence of any firm guidelines, I think the safe and prudent path is to take it on a case by case basis and work closely with the cardiologists/cardiac nurses. I also think there is an element of trial and error in easing the patient into resistance training and evaluating their tolerance to it. Everyone is looking for cookie cutter “guidelines” but the operative word is “guidelines” and not the end-all-be-all this is the way it MUST be done. Thanks for your comment.
My husband had defribullator surgery. March 13th. His primary cardiac physician thinks he needs at least two more weeks before he returns to work. The surgeon who implanted the device says he can return now. What concerns me is I think both doctors fail to understand that there are a battery of tests he must pass in order to be allowed to return to work. One involves fully extending his left arm and his right leg and then pulling his full body weight in a crawling position. He must do ten reps of this exercise. I feel that just a bit over a month after his surgery, especially after his doctor explained to me how critical it was that the leads not be pulled loose even one millimeter, or another surgery would be necessary, that someone is not understanding the gravity of the situation. My husband weighs 250 lbs. I think that is a bit too much weight for him to be pulling with his left hand in an overhead crawl at this point. Is the doctor just not getting it, or am I being overly protective?
Hi Theresa,
You are justified in being concerned and you must always be a strong advocate for yourself and the people you love. How is your husband feeling now five weeks after the surgery? Has he tried any of the movements he’ll be required to do for the test? And if so, how did he fare? I think it’s wise to work closely with both the doctors and perhaps a clinical exercise physiologist from your hospital’s cardiac rehabilitation department (if they have one). I think getting a few heads on board will help allay your fears and help your husband transition back into his work role. Please let me know how you go with all this by leaving a follow up comment or send me an email. All the best.
I am 31 years old and had an icd installed January 20 due to genetics that can cause sudden cardiac death and I have a heart block. I was an avid exerciser before and ran at least 5 days a week. I like to do half marathons and triathlons. After the icd, if I do anything that raises my heart rate above 150, it will just keep racing until my icd goes off. The first time it went off I was walking on the treadmill. The second time it went off I was trying to play basketball with friends and got shocked 3 times and the third time I was walking on the treadmill and got shocked 4 times. All times my heart rate got above 230. My question is what is a safe rate to get my heart rate up to because I am tired of getting shocked.
I should add that all the shocks are said to be inappropriate because they came from the top chamber
Hi Marsha,
That is a great question and one which really doesn’t have a simple answer. The best answer to these types of questions is always the same: It depends. What might be a safe heart rate for you could be inappropriate for someone else, and vice versa. The best thing you can do in this case is speak to your cardiologist in depth and explain the situation. It is affecting your quality of life everytime you get a shock so clearly this should be investigated in order to find some sort of resolution (as soon as possible). I apologise for not being able to give you a finite answer, but my training is as a clinical exercise physiologist and not a cardiologist. You would, however, benefit by including an exercise physiologist as part of your treatment plan to work in partnership with your cardiologist. I think that will give you the best chance of getting all this under control. Stop back and leave another comment once you speak to your heart team. Kind regards, Bill
You shroud talk to your doctor. I had the same problem, genetic heart condition, avid exerciser. My cardiologist put me on betablockers so my heart doesn’t get out of control so easily. I’ve had the ICD for 18 months and have been exercising/running 5-6 times a week for 1 year. Is a lot harder to run on beta blockers but is much safer. No shocks so far!!
Marsha , hi my name is Chris and it sounds like we suffer from the same . Although they call it sudden cardiac arrest lol. Shoot Ive been shocked and have passed out with the ICD . I’m not looking forwrd to working out to get back in shape ,but we must forge on, not go quietly into that goodnight. We just have to be real carefull . I will be . Best of luck.
Hi Bill,
Just found this site and discussion and at last feel I have found someone able to understand and discuss the risks and methods of getting back into regular healthy exercise.
I am a 56 year male. Last year was diagnosed with bradycardia and had pacemaker inserted, this go infected and had it moved to right hand side. 3 months later serious arythmia and defibrillated followed by cabg surgery. A couple of months later another arythymia and had icd implanted.
Now I find myself struggling to develop and stamina. Up until 50’s was consistent exeriser including masters squash, weightlifting, skiing, golf and cycling. I have recently retired to look after my wife who has alzeihmers and am struggling to develop a regular training routine as I am lacking confidence in how hard to push myself. On walks of up to 7km at approx 6kmh my heart rate is 110-120 which is what I used to do when jogging. I would like to get back to spinning classes but scared on hiit training sending me into arythmia or shock.
Any suggestions on appropriate training methodologies I could discuss with my electrocardioligist.
G’Day Wayne,
Thanks for taking the time to write and share your story. Whilst I cannot give you any specific guidelines over the internet (since I’m unfamiliar with your detailed medical history), I would suggest discussing the following questions with your cardiologist:
1) Was there any evidence of a heart attack (myocardial infarction) with/without heart muscle damage? I’m guessing not based on what you wrote, but it’s good to be thorough. I’ve had clients who were unaware they had a heart attack.
2) What medications are you on and how will these impact your ability to tolerate higher intensities? Sometimes you can have all the desire to exercise in the world but medications can suck the wind out of your sails.
3) Which arrhythmias did you experience? Were they atrial or ventricular arrhythmias? Usually the occasional premature ventricular contraction (PVC) is no big deal, but if you get long runs of PVCs where you become symptomatic, then you definitely need to see your doc.
4) Discuss the settings on your pacemaker and ICD with your cardiologist regarding the triggers that will set them off. I would specifically discuss your desire to do higher intensity spinning classes again and what the risks are to your specific situation.
All in all, I think it’s important to be very familiar with your particular health conditions and the limits settings on your pacemaker/ICD in order to know what you can do. Make sure it will not deliver a shock under normal circumstances even if you happen to reach a higher heart rate. I’ve worked with a lot of ICD patients in my cardiac rehab program and if they were properly managed they were able to live a reasonably normal life again.
Hope this helps, Wayne. Take care and feel free to leave another comment after you’ve been to see your cardiologist.
Kind regards,
Bill
Dear Dr Sukala,
=> Would it be safe to be UNDER water/on the beach/in the low surf, just standing/sitting there, or some form of very limited activity, maybe yes/no, limited body surfing mindful of the leads?
All very nice and easy; love the beach.
Had ICD p/maker/defib implanted 6/52 ago post cardiac arrests/myopathy.
On various cardiac medications now. Potential s/effects re sun/UV.
Used to be regular/fit exerciser.
Starting again. Walking.
And:
=> Bicycle soon: have you heard if an e-bike is safe to use? Like a mixture of a bicycle with a scooter, based on Li battery driven electromagnetic motor? No driver’s licence required.
Thank you for your reply in due course.
Hello Heinz,
Thank you for your comment. I’m not quite clear on when you had your ICD implanted, but provided your surgery wasn’t too recent, then you should be ok to go in the water (once you have received clearance from your doctor). In the early post-op phase, you’d have to be very careful with the lead wires and overhead movements. Here is a quick link which may provide some extra helpful information: https://www.mayoclinic.org/tests-procedures/implantable-cardioverter-defibrillators/details/results/rsc-20206182
Regarding the bicycle, I have heard of these types of bikes. Talk to your doctor about the heart rate limits set on your ICD to make sure it does not deliver you a shock when your heart rate rises normally with exercise. I think the newer models are better than the older models from years ago, but always best to check with your doc to be sure. Provided your heart rate is not going to climb too high, the bike probably wouldn’t be too much of a concern. But again, the final word should come from your doctor, as he/she is specific with your individual medical history and surgery.
Hope this helps.
Warm regards,
Bill
Hello
In January 2014 I had a cardiac arrest whilst exercising on my bike at home and diagnosed with arrythmia, hence and ICD was fitted. The arrest was totally out of the blue and I have had no previous heart problems before or family history. I am now taking mg of bisoprolol beta blocker a day and feel absolutely fine and have regular check ups. There has been no problems since. I ave been told that any exercise that is over 130 beats per minute is not acceptable and only walking is good for me. This I find frustrating as I have put on 7 kilos over 2 years and as being used to exercise, I do feel very low about this at times. Also do I have to stay on beta blockers for ever?
Hi Julie,
I can certainly understand your frustration. I would suggest speaking to your electrophysiologist (cardiologist) to discuss the ICD limits. Find out what the max heart rate is based on the ICD settings and if it is able to distinguish between elevated heart rates due to exercise (normal sinus tachycardia) compared to runs of ventricular tachycardia (the bad stuff). The beta-blocker is obviously meant to keep your heart rate down at levels low enough that the ICD doesn’t give you a shock.
Having said all that, I can’t legally comment or give specific medical advice because obviously I’m not aware of your entire medical history and I’m not a cardiologist. I would suggest having another “heart to heart” (pun intended) with your cardiologist about these issues and see if you can work together (within the confines of your particular condition) to lower your beta-blocker dose, adjust your ICD limits, and allow you to get back doing exercise at a comparatively higher intensity that will help you lose weight.
I hope this helps.
Kind regards,
Bill
Hello,
This is a nice article for guidance on exercise with an ICD. Very helpful!
I received an ICD on February 4th 2012. 2 days before I suffered sudden cardiac death but was saved by several awesome people and an AED. I was 39 at the time. The root cause has never been identified even with genetic test. I went back to basketball and working out 4 or 5 days a week with no problems until Jan. 4 this year. My ICD shocked me 3 times (brutal) over an hour long period before I could get to the ER. Turns out the leads had fractured and a short caused the 3 shocks. My ICD was replaced. I backed off the amount and intensity of my exercise but still made it 3 days a week, no more basketball though. But, on August 20th this year, my ICD shocked me 5 more times. I was on a stair master at the gym. The Dr.’s and device techs all tell me it did what it was supposed to do on the first one (my heart beat was headed into a VFib again) but the other 4 were because a lead had moved so it was somehow misreading something. I find it hard to believe the lead misplacement didn’t help cause the initial rhythm/s but I’m not an EP so I have to go with what they say. I’m trying to put all that behind me and wanting to find some level of exercise that won’t increase my chance of another inappropriate shock. I was thinking yoga would be a good start with some bike for cardio. You mentioned yoga irritating the implant site…is that after recent surgeries are at anytime with an ICD? By irritation do you mean it’s an odd sensation or causes some swelling and pain?
Thanks!
Hi CP,
Thanks for your comment. I was just making a general comment regarding exercises which might affect the ICD, be it just after implantation or beyond. Anything that could affect the wires or bump the ICD needs to be carefully controlled (which applies to yoga as well). On that note, I think yoga is a good idea, but you’ll want to be careful. I’d suggest speaking to your cardiologist or the cardiologist’s practice nurse and discuss your concerns. Hope this helps. Cheers, Bill
This is the most intense article I have read about the defibrillator.
Thanks
Thanks. I wasn’t trying to be intense, but I guess I’ll take that as a good thing 🙂
Hi Bill,
Great article, really informative, I had an ICD fitted back in 2015, but I now want to start keeping a bit fitted due to aging. I have been lifting some light weights, and don’t push ups and sit ups. Had no real problems, but I want to start using a rowing machine, what would be your advice here please?
Regards
Steve
Hi Steven, Thanks for your comment. The prudent course of action would be to speak with your cardiologist to make sure it won’t affect your ICD. If given the all clear, then you might want to start out easing into it with a few shorter/lighter sessions and see how you feel. If no problems, then gradually increase both duration and intensity over time. Your cardiologist can advise you if there are any risks around higher heart rates and if your ICD will deliver a shock due to elevations in heart rate due to exercise versus an arrhythmia. As long as you keep in close contact with your cardiologist and have clear communication and understanding about your ICD settings, chances are you’ll probably be just fine. Usually the people who have problems are the ones who decide to go out on their own and start blasting themselves into oblivion with exercise. Bottom line: always better to be safe than sorry and cross your T’s and dot the I’s. Best wishes
Hi. I was diagnosed with dilated cardiomyopathy in 1989 and was suffering VT upon exercise (I was a triathlete). Following medication (beta blockers and anti-arythmic drugs) I had a lay off period of about 6 months but gradually started exercising again to the point that I competed in triathlon and adventure races again. I had two cardiac ablations in the 1990s. I have remained active since, albeit now just cycling (enduro MTB and road riding with a local club). September last year, following a cardiac MRI, I was told that I have ARVC and should stop all exercise and recommended that I have an ICD. My consultant didn’t really want to engage a conversation about my riding to HR threshold level and I got the impression that anything other than light exercise was a no no. I have been largely inactive since then (apart from walking the dog and a few gentle short rides )and am due to have the ICD fitted in a weeks time. I had pretty much thought my cycling was over but am now wondering whether I might be able to ride an eMTB. I demo’d a few bikes today and found my HR was still up 150+ at certain times. So I am wondering whether continuing riding eMTB is a possibility post ICD? Or is the issue more one that this sort of exercise level will be too “extreme” in any event and aggravate/compound my ARVC? Thanks in anticipation.
Hi Daron,
Whilst I can’t give any specific advice, I can certainly suggest some things you may wish to discuss with your cardiologist. When it comes to your heart, better the devil you know than the one you don’t know. Dealing with these health issues is certainly a serious concern, but at least they’re out in the open with a spotlight on them. First things first, get your ICD fitted and then talk with your doc about the HR limits programmed into the device. The best thing you can do is be honest with your doc and try to work together to address your lifestyle issues as well as the safety aspects around your physical well-being. In most cases, there will be a bit of a “settling in” period while you get accustomed to the ICD. To be honest, in working with cardiac patients, I’m much more vigilant of the person with arrhythmias WITHOUT an ICD than I am the person with arrhythmias WITH an ICD. There might also be some concerns about the jolting effect on your body associated with mountain biking, but again, it still comes back to the basics. Discuss it with your doctor and try to find ways that you can both take care of your health and also address your concerns around staying healthy and fit. One thing we do know with absolute certainty is that, yes, all exercise has risk associated with it, but doing zero exercise is far worse for you than assuming some risk in doing exercise. Bottom line: Get the ICD, make sure you understand your device’s setting’s, and what the ramifications are for you taking up exercise.
Cheers,
Bill
Many thanks for the prompt response Bill. I can certainly see the issue with the jolting effect and I am thinking that perhaps my hopes were a little optimistic. As you say, I’ll speak to my cardiologist and go from there. Regards
Daron
Cheers Daron, I definitely wouldn’t say to accept defeat. It’s just a case of working closely with your cardiologist. With the ARVC, it’s a case of better the devil you know than the one you don’t. Feel free to stop back and leave some more comments because your experience might benefit others going through something similar. Cheers
Hi Dr Bill
I’m a 73 yr old Canadian female originally ICD implanted 10 years ago – now on #3. Congenital LQT type 2 caused vtach, vfib and arrests. Cardiologist recently warned of danger of device erupting through skin of chest.
I take regular exercise classes with cardio, 2 lb weights and flexibility.
Where would I find what kind of exercises to avoid chest muscles moving the device beneath the skin?
Thanks for taking the time to give advice to one of what my friends call “a bionic woman”.
Hi Jayne,
I don’t think there’s any cookie cutter approach to this since each person’s situation can be a little different, but I think a wise and prudent course of action might be to find a cardiac rehab program in your area (are you around Ontario?). If so, check out this website from the Cardiac Rehab Network of Ontario for more information: https://www.crno.ca. If you can work with a clinical exercise physiologist or physical therapist with experience with ICDs, then they can give you personal attention and help you find the best exercises for your individual situation.
Bottom line: as a general rule, there are always ways to exercise no matter what health challenges get in the way. Once you find them, then you’ll be well on your way back to good health (and feeling good about it too).
Kind regards,
Bill
Hi bill
I have a defibrillator also
The problem im sitting with is that I dont have any medical aid no more. Im not working and cant afford my tablets anymore
I was rushed to groote schuur hospital and was there for almost 11 hours with just laying on a bed
I dont know who to deal with according to my conditions and I am also unemployed
Can you please assist I really need help and when I was on medical aid I could afford it but now im unemployed and its sad
Hi, I went into cardiac arrest in a cardiologist office (I know-very, very lucky). I recently had catheter ablation performed and have a implantable cardiac defibrillator. I am 28 and an elite runner. I am qualified for the 2020 Olympic trials in the marathon. Should I even consider continuing the necessary training required to compete for a place on the USA team (prior to this happening, it was not inconceivable).
I understand that my cardiologist is the final word, but I would like your thoughts on this. Thank you
Hi John,
Wow, that’s quite a story. And yes, you were lucky that it all went down in your cardiologist’s office. I think the answer to your question would probably depend on 1) what caused the cardiac arrest; and 2) the extent to which this is now managed. As a general rule, it’s a question of whether or not prolonged exercise might worsen your condition. Obviously we know exercise is a good thing, but even at high/prolonged “doses” it can sometimes throw things a bit out of wack. You might want to ask your cardiologist (electrophysiologist) if 1) training at the levels you’re intending could plausibly affect your condition; and 2) are there settings that can be adjusted on the ICD to allow you to safely train and compete? In closing, I’ll say this: I have worked with a number of elite athletes who’ve had multiple heart attacks and were still able to train and compete but, admittedly, not at the Olympic level. Still, never give up hope and throw in the towel. Yes, it’s serious sh*t, but sometimes better the devil you know than the one you don’t know. Imagine if the cardiac arrest had happened while you were out training on a quiet road with no one around. I’m not happy this happened to you, but at least your proverbial volcano erupted now and not at a worse time. I’d love to give you an answer but as you pointed out, only your cardiologist can give the final word given that he/she will be most familiar with your entire medical history. Kind regards, Bill
Hello Dr Bill. I had a pacemaker fitted 2 weeks ago and want to return to weight training and cycling as soon as possible so as not to lose hard fought conditioning (I am 77 yo) pm fitted because heart rate dropped to 27 whilst sleeping 164 times but each time I awoke hrs returned to 50+_. Hasn’t assisted as yet. Which exercises should I not be doing have been told elbows not to go above shoulder. Also could you recommend and exercise physiologist on the northern beaches. Thanks Keith
Hi Keith,
Thanks for your comment. As everyone is unique, I can’t give any specific advice. Probably best to have a proper and focused conversation with your cardiologist about exercise and what might be best indicated for your individual situation.
For the patients I’ve worked with that have bradycardia (slow heart rate), they’re not as critical from an exercise standpoint as those with atrial fibrillation that suffer from extremely high heart rates. Does your heart rate climb normally with exercise and tend to recover normally after exercise?
Regarding your elbows not going above your shoulder, this is likely to be due to the recent placement of the pacemaker. Ask your docs what the restrictions are for you after a month or two once it has “settled” so to speak. They’ll probably just tell you to ease off the blood sports and footy!
You might try contacting the team at Royal North Shore Hospital, as I believe they have a cardiac rehab program there. They can either help you directly or perhaps point you in the right direction to someone on the northern beaches with experience. You might also contact a colleague of mine Andrew Sumner who is an exercise physiologist and physiotherapist based up around Mona Vale. Tell him I referred you. He’s a really good guy and, if he can’t help you, he can point you in the right direction as well. Hope this helps. Cheers, Bill
Thanks for prompt reply Dr Bill will follow up and report back on results. Stay well Keith
Dr. Bill. Hello I had my icd implanted in June 2016. I am an active golfer and was 37 at the time it was implanted. I never had an issue all my checks came back great and everything was fine. Then on November 10, 2018 I was getting ready for friends to come over to watch football for the day. My device malfunctioned and shocked me 18 times in 35 minutes. Sometime between my last device check and the this time my one of my leads became fractured. The lead which was fractured was left in but was disabled. There was reason given to me as to why my lead fractured, and after reading i was worried it maybe because of the amount of golf I play. Now I am worried the disabled lead that was left in will run against the new lead and cause it to fracture as well, especially if I play golf as much as I always have. I guess my question is… is this all in my paranoid mind? Can I continue to be an avid golfer with no worries? My life the past few months has been filled with anxiety and fear. I just want to hit the links and not be worried I am causing damage as the same time
Hi Teresa, Thanks for your comment. I can imagine that would be quite anxiety-provoking after going through all that. I can’t give any specific answer since I’m not directly involved in your care, but I would strongly suggest having a talk with your electrophysiologist who should best be able to help you. Depending on how aggressive your movements are around the chest and shoulder girdle, this could theoretically cause issues but, again, your best bet is to get more detailed information from your cardiologist and discuss the movement patterns that you go through when playing golf. I have worked with a number of people with ICDs and it was just a case of figuring out what modifications to make to best accommodate their condition. Hope this helps. Kind regards, Bill
Hi Dr. Bill. I’m a 51 year old man, I was an avid recreational runner, completing 5 marathons, 1 a year over the las t 5 years (finishing in 4-5 hours) . I also did high intensity workouts at a specialty gym. (Orange Theory). After an episode of a-fib, I was diagnosed with non blockage HCM. Because there was some non sustained ventricular tachycardia after wearing a monitor, and an incomplete family history, I had ICD surgery in December. As others have stated, my cardiologist and my team at the HCM center will not give me any specific guidance on exercise. I’ve gained 45 pounds since the a-fib. I’m on beta blockers and blood thinners. I would like to return to running, possibly as far as 10k, but I’m confused about the effects of running. Any advice would be appreciated.
Hi Bill
Thanks for your comment. Wow, it sounds like you’ve been through the wars with all that happening. Hypertrophic cardiomyopathy is serious business. Did your docs give you any indication about what might have caused the HCM in the first place? Atrial fibrillation is no fun but that is something that tends to be manageable in most cases. The run of ventricular tachycardia can also be quite serious depending on how long the runs are and if they do not resolve on their own. VT can convert into ventricular fibrillation (which is really bad). So looking at everything you’ve said, the ICD is probably the best option moving forward.
I’d also point out that since your ICD surgery was in December, it’s still somewhat early days. Whilst I can’t give any specific exercise guidelines since I’m not part of your medical management team, I can perhaps provide you with some suggestions that you can discuss with your docs and allied health professionals involved in your care.
1) Regarding exercise, I would suggest speaking to your docs about getting a referral for cardiac rehabilitation (particularly one that uses continuous telemetry monitoring). Based on your IP address, you look to be in the northeast US. The US is quite good about cardiac rehab compared to overseas (I’m from the US so I’m aware). Cardiac rehab will give you an opportunity to exercise under safe and controlled circumstances and have a team there to guide you. You’ll need to have your doc and the cardiac rehab team work together to talk about safe endpoints for your heart rate and blood pressure. And also work with what’s known as the rating of perceived exertion scale (RPE) because you are on beta blockers and your HR and BP response will be blunted. Over time, you will start to identify the workloads that are both tolerable and without signs or symptoms (or ectopy on the ECG). The more information you have from your cardiac rehab sessions, the better to help you plead your case to your doc about safe exercise guidelines.
2) Regarding the 45 lbs you gained, this could probably be explained by your being less physically active due to the heart issues. You might consider getting a referral to a registered dietitian to help you with your eating and help intervene through dietary means while you’re getting your exercise sorted out with the cardiac rehab team. In some cases, the cardiac rehab team works with dietitians too, so you might get a two for one in that case depending on the CR program.
3) As I said above, this is all serious stuff you’re going through, so if you’re feeling a bit anxious (as would be normal in this case), I would also suggest speaking to a social worker or psychologist from the hospital who has experience working with people dealing with medical issues. I can tell you with reasonable confidence, it will be very helpful to balance out all the thoughts and feelings you’re dealing with. In particular, very active people tend to have a harder time when the doc says things like “no exercise.” It’s a part of your life and to have it cut out virtually overnight is a kick in the balls. So while you’re trying to deal with getting your exercise and nutrition sorted, it also helps immensely to get your head space under control too.
Bottom line: find out what the underlying cause is of the HCM. Know your ICD settings and what that limits are. Attend cardiac rehab (if approved by the doc) and work closely with the team using continuous telemetry monitoring to tease out appropriate workloads, heart rate and blood pressure responses, and your rating of perceived exertion (RPE). Putting all these things together will give you a treasure trove of info that will guide you moving forward. Hit up the dietitian and social worker/psychologist to get your headspace under control (if you feel this is getting to you). Remember this final pearl of wisdom: reaching out for help is a sign of strength, not weakness. You’re still in early days since your ICD and this is an adjustment. When I use to see people in cardiac rehab with an ICD, I was much more relaxed than those with serious arrhythmias without an ICD. It’s sort of an insurance policy in case things go bad. In other words, sometimes better the devil you know than the one you don’t know!
Hope this helps. Feel free to stop back and post a follow up so others can benefit from your story. I’ve also removed your last name to protect your privacy.
Kind regards,
Bill
I’m a competitive bodybuilder and personal trainer I know competitions is over but what about weight lifting to stay in shape. Also I still take 0.5 testerone from my doctor with a little extra. Should I stop everything
Hi Steven,
If you recently had an ICD placed, then there’s a bit of a learning curve in getting back to exercise. As I said in my response to Bill R in a different comment, I would strongly suggest getting a referral to a cardiac rehab that uses continuous telemetry monitoring. They can help guide you and check out your ticker at different workloads to see how you tolerate exercise. Provided you can tolerate higher aerobic exercise workloads without any ectopy, then you might discuss with your doctor the possibility of lifting weights. You’d have to use common sense rules such as easing into from lower weights in the beginning to higher weights and monitor for signs and symptoms (and ectopy on the ECG).
Bottom line: work closely with your cardiologist and see about getting a referral to cardiac rehab for closer monitoring at different workloads. After you have some data to work with, then speak with your cardiologist again with this information in hand and see if you can workout a mutually agreeable plan moving forward. Also discuss your ICD settings and at what workloads your ICD will give you a shock (and if it can differentiate between an increase in HR from exercise versus an arrhythmia).
Hope this helps
Bill
Hi Dr. Bill, thank you for your help.
I have icd implanted 18 days a go and I’m experiencing difficulties during slight slope up gradient walks. Will conditions improve? I used to be cross country runner and
heart rate in the 40s. I’m HCM patient. What should I do to get back to my usual activity?
Hi Joseph, thanks for taking the time to leave a comment.
Since you’re still pretty fresh out of your ICD placement procedure, I’d suggest talking to your doc about getting a referral to a hospital-based cardiac rehab program (ideally one that uses telemetry monitoring). Assuming they have clinical exercise physiologists on staff, they can help you work through different levels of exercise and closely monitor you every step of the way. This information can be used to inform your discussions with your cardiologist about getting back to your usual activity.
I can’t give you any specific info but I would strongly recommend working closely with your cardiologist and discuss your previous exercise history and any concerns you might have. Hope this helps.
Kind regards,
Bill
Hello Dr.Bill,
I followed your advice, and increased my walking to pre implement condition. I walk now 6-7 miles with 16 minutes a mile rate. Thank you for your advice.
Pre implant I sometimes get close to fall, faint when I during running. It happens with palpitations and feeling dizzy. Now after icd planted, I was thinking things will improve but unfortunately I feel dizzy when I run. I take calcium channel blocker for high blood pressure.
What should I do Dr.Bill to avoid dizziness during running and run with out fear. I love to run but now I stopped running. I love to get back on running.
Please advise me what to do Dr. Bill
This I
Hi Joseph,
Thanks for your question. I would recommend speaking with your doc about your blood pressure and BP medications. If the meds are working a little bit too well, then they could plausibly be causing your blood pressure to drop too low. Remember that when you become active, your blood vessels dilate to accommodate more blood flow to the working muscles (which is desirable). But when you stop exercising, your blood vessels remain dilated and, in combination with the blood pressure meds, you might experience some sort of compounded effect which causes your blood pressure to drop very low. Clearly you’re having symptoms, but you’ll definitely want to get to the bottom of things so you can get back to living life normally again. If these symptoms are brought on during exercise, then you might ask your doctor if a stress test is appropriate so they can check out your response to graded exercise. If they can reproduce the symptoms, then they would have a better chance of pinpointing what’s causing it. Hope this helps, Kind regards, Bill
Hello Dr. Bill,
Thank you for your prompt response and advice. I live in the middle of nowhere ( in the mountains of Wyoming) where I could access any rehab facility.
But my walking is improving now at all levels of slope gradient.
My question to you is how soon do you recommend me to start slow run or jogging? I’m on my third week after the dual chamber abbot icd implant.
Thank you so much for your advice.
Hi Joseph,
I can’t actually give you any specific guidelines since I don’t have any involvement in your care. Your doctor is really the only person you should trust with an answer to that question. If the implant was successful and the docs deem it stable, then they may give you permission and/or guidelines specific to your situation. On a side note, I’ve seen a number of tele-cardiac rehab programs where you can work with a rehab team remotely and get specific customised advice in partnership with your medical management team. Might also be worth asking your doc about something like this. Kind regards, Bill
I’m a 69 yo female with an ICD implanted 5 weeks ago. Last week the atrial lead dislodged and will be fixed in 2 weeks. I am a 10 mile a day bicyclist, walk 2-3 miles a day and use aqua barbells in the pool as my primary exercises. I am 5’10”, 145 lbs and in good muscle tone. I just started riding again last week and have been walking regularly since the procedure. I have stayed away from the aqua barbells and arm exercises with exercise bands because I am concerned about movement of my left arm. After the repeat procedure to fix the dislodged lead, what arm movement exercises will be safe to do to avoid subsequent dislodging of the leads?
Hi Sandra,
Speak to your doctors for specific guidelines. In general, the best advice is to limit arm moments on the side of the ICD for anywhere from 2 to 6 weeks, but that really depends on your individual situation. Have a conversation with your medical management team and ask what would be appropriate in your case. Kind regards, Bill
Great logical advice…glad I found your site.
Hi Dr. Sukala,
I’m 33yrs old and had an ICD placed about 5 months ago. Prior to placement, I was very active and would do around two sets of 10-15 pull-ups and 25 push-ups 4 to 5 days a week.
I’d like to get back to these activities, though I fear breaking a lead from the repetitive movement under stress.
Could you share your perspective on the risk of breaking leads while engaging in the activities? Would narrow vs wide grip/position make any difference? Should I expect the leads to wear out and break eventually regardless of my choice in activity?
Thanks in advance for your time, and for this article!
Jackie
Hi Jackie,
Thanks for taking the time to leave a comment and for your excellent questions.
As with any electrical device, an ICD will experience normal wear and tear over time. Any exercise that causes the wires to repeatedly flex could plausibly lead to greater wear and tear and contribute to it wearing out sooner. I would strongly suggest having this conversation with your cardiologist and discussing your needs regarding exercise. It is definitely a quality of life issue for you so it’s a worthwhile discussion. You might also want to discuss what the usual lifespan is of the device and how often the wires would need replacing under normal circumstances. The more information you have in this regard, the better off you’ll be with keeping up with any potential maintenance.
The other consideration is that aggressive exercise could plausibly affect the lead placement and cause it to dislodge. But again, these are all points worth brining up with your cardiologist (or if unavailable, speak to the practice nurse). Good quality information is going to give you the peace of mind you need to exercise safely. Over time, you’ll get a better indication of what exercises are safer than others with regards to the leads.
Hope this is helpful. Feel free to stop back and leave another comment.
Kind regards,
Bill
How soon after an ICD implant is it safe to take a full hard golf swing?
Hi Marty,
It’s hard to say exactly. I would strongly encourage you to discuss this with your cardiologist who will best be able to give you a firm answer.
Kind regards,
Bill
Hey I hope you’re still answering comments! I haven’t got a straight answer for this yet. My issue isn’t with the physical strain from the exercise, my worry is what weight lifting exercises will strain or potentially break the leads? Do I stay away from chest exercises? Push-ups? Any lifting over my head like shoulder press? I’ve been told to stay away from repetitive chest movements but no clear defined answer
Hi Joshua,
Thanks for taking the time to leave a comment. I don’t think this is one of those cut and dry yes or no sorts of situations, but one in which you need to work closely with your cardiologist in order to work out the dos and don’ts specific to your situation. If you were doing highly explosive exercises like Cross-Fit, then that could plausibly affect the leads more so than controlled movements with a stable upper body. There may be wear and tear on the leads so this could be a concern, but it’s about working with your cardiologist and discussing the quality of life issues versus the (obviously) important placement of the ICD. Moving forward, it will be important to know the standard life span of the ICD and wires in order to plan for replacements along the way. Feel free to stop back with any updates or questions so that other readers may benefit.
Kind regards,
Bill
I’ve been looking for information on safety exercising with an icd for a long time. This is the first time I’ve found anything even close to what I’m in need of.
I’m so confused. When I first got my icd I was told that I could never use my bow flex again. That it would bend my leads. Is this true? My arms went to crap! They haven’t had any exercise for 4 years now because I was afraid I’d break it.
Thank you!
Perhaps take a short video clip of how the machine works and then send it to your cardiologist to assess if it will affect your leads. Also bear in mind that exercise intensity may also affect the impact on the wires. It may be in your best interest to attend a cardiac rehabilitation to see about getting an assessment with an exercise physiologist and finding some exercises that will do the job and also be appropriate for your specific situation. Hope this helps.
My nurse that reads my pacemaker told me I can’t have my clavicle go over my first rib because it may cause too much wear on my lead. What exercise can I do at the gym and what should I avoid?
Hi Richard, I’d recommend talking to your cardiologist to see about getting a referral to your closest cardiac rehabilitation. They will be able to work closely with you in a controlled environment to help you find the exercise motions that will be safe and not impact your leads. I’m sorry I’m unable to be more specific here, as I’m not able to give any specific advice online. Your medical management team will be most familiar with your medical history and will best be able to help you. Kind regards, Bill
Hi great questions and information. I am 73, icd implant in 2004 and starting to return to the pool for exercise. Doing 1300 yards in my 45 minute session, my question involves trying to increase my session work load (faster, farther) on beta blocker and having trouble becoming out of breath during hard swims. In your experience should I keep pushing and will I enlarge my heart by harder training ( had heart damage from heart attack) thus the icd. Thanks
Hi Bill
Thanks for your question. Regarding increasing workload while on a beta-blocker, this is a tricky one. Up front, my disclaimer is always to work closely with your doctor who will be most familiar with your entire medical history. With that, you might which to discuss the dosage with your doc and ask if it’s appropriate to lower the dose or perhaps find other meds which might be appropriate that do not have the same degree of heart rate-lowering effect. But it’s also important to remember that even with a beta blocker, it’s possible to derive benefits to your heart muscle. I’m not inclined to think it will necessarily enlarge your heart in a bad way, but it my result in a thicker and stronger left ventricle (which is a normal and expected adaptation to exercise). Also, as for the ICD, it’s actually a good thing that you have one in place because if your heart converted to a dangerous rhythm, the ICD will detect this and deliver a shock to buy you some time to get it checked out. I’m much more afraid of the person who has had a heart attack and does NOT have the ICD in place! Hope this helps.
Kind regards,
Bill
Thank you for your article. It answers many of my questions, I got my ICD implanted last week. I feel like a new man. I m already going for walks and I m looking forward going back to gym. I really enjoy lifting weights. Nothing excessive though. I plan to start with legs and in three weeks will start upper body .
I feel like a brand new man. My EF was 25, I m 62, and I have always been very active. All my heart issues started in the last two years, but worsened last year.
Thank you for your article.
Hello Dr Sukala,
Greatly enjoyed your article and all the comments. I will be getting an EV-ICD (extravascular ICD) with no leads planted in the heart but with the sensor placed under the sternum and generator placed to the side axial. I was wondering your thoughts given its potential benefits (no leads in the heart, less restriction of motion as no leads are in danger of fracture etc. with any downsides that as an expert might perceive.
Hi Trellis, the EV-ICD may be less visible and more comfortable than other standard ICDs. They tend to send small electrical signals to correct your rhythm before delivering a shock. Potential downsides are not unlike a standard ICD and may include lead dislodgment, inappropriate shocks, or the risk of the EV-ICD entering the pericardium, pleural space, or abdominal space. As with any cardiac procedure, work closely with your cardiologist and follow the recommendations for your specific situation. Cheers 🙏