What is atrial fibrillation?
Before I explain what atrial fibrillation is, it’s important to understand that normal electrical signals in the heart are timed so that the chambers beat in a coordinated rhythmic fashion (called normal sinus rhythm).
Blood from the top chambers (atria) is transferred down to your lower chambers (ventricles) and then pumped out to your body to meet oxygen and nutrient needs.
Atrial fibrillation (also called “a-fib”) is a common condition that occurs when there is a “short-circuit” or disruption in the heart’s normal electrical conduction system, causing the atria (upper chambers) to beat in a rapid and irregular manner.
With a-fib, the atria beat as fast as 300 to 600 beats per minute.
The atrioventricular node, which normally transfers the beats propagated in the atria down to the ventricles, serves as a buffer and fortunately does not conduct all these impulses in the ventricles.
Irregular heart beats alter the normal flow of blood through the heart’s chambers (from top down), causing incomplete filling of the ventricles and a reduction in your heart’s ability to pump oxygen and nutrient-rich blood to all parts of your body.
Signs and symptoms
Some people may have no overt symptoms, particularly if their atrial fibrillation is transient and each episode is short-lived.
Symptoms can range from palpitations (the feeling like your heart is fluttering in your chest), shortness of breath, chest pain, dizziness or fainting spells, weakness, or confusion.
If you think about it, these symptoms make sense.
With atrial fibrillation, your heart muscle is not pumping out enough blood (due to inadequate filling of the ventricles), and without adequate oxygen getting to your brain, lungs, muscles, and other target organs, it’s only logical that you should feel lousy.
A stroke is another concern with a-fib.
It is possible that blood can pool inside the heart, giving rise to a blood clot (thrombus) which, once it breaks off and exits the heart, floats around your circulatory system as a clog waiting to happen.
If it ends up in the brain, then you have a good old-fashioned stroke.
This is precisely the reason why blood-thinning medications like warfarin and aspirin are important
Short video on atrial fibrillation and stroke risk
If you learn better from online videos, I found this short clip on atrial fibrillation and its role in stroke.
Causes of atrial fibrillation
In some cases, the cause of atrial fibrillation is unknown.
But in most instances, it occurs in tandem with other health conditions such as hypertension (high blood pressure), previous heart attack, valvular defects, congestive heart failure, or associated comorbidities like obesity.
In my experience working in hospital-based cardiac rehab, it is not entirely uncommon to see a-fib patients after open-heart surgery , heart valve surgery, and angioplasty/stent (particularly after a heart attack).
Treatment options
You should understand that atrial fibrillation is not the end of the world.
Your cardiac specialist will need to run some tests (such as an electrocardiogram or ECG) on you to ascertain how severe (or not severe) your condition is.
In many cases, it can be treated with anti-arrhythmic medication and blood thinners (see stroke risk above).
Other approaches entail using cardioversion to “jolt” the heart back into normal rhythm, or catheter ablation to isolate and zap the specific region of the heart that is the source of the atrial fibrillation.
Exercise guidelines for atrial fibrillation
I am often asked for “right-wrong” or “black-and-white” guidelines for safe exercise with atrial fibrillation, but the short answer is always “it depends” on the individual circumstances.
A-fib often presents in concert with other underlying health conditions, so the exercise prescription cannot be a one size fits all approach.
To follow some random exercise program off the internet could leave you face down and unconscious on the pavement while taking your afternoon walk!
Having said that, the good news is that you CAN exercise safely with atrial fibrillation.
Have a detailed discussion with your cardiologist and medical management team and find out if there are any specific considerations that would preclude you from doing any certain types of activities.
If you were previously active, then you should let them know what your previous regimen was and what you’d like to achieve now after your diagnosis.
Because the condition can reduce how much blood is ultimately reaching your exercising muscles, you will likely need to start off at a low level and then gradually increase your intensity and duration as tolerated.
A heart rate monitor “may” help you, but the inherent problem is that the numbers might jump around a bit with an irregular heart rhythms.
The most prudent advice is to consult a clinical exercise physiologist with experience working with people with cardiac conditions.
Aerobic exercise guidelines
You can perform aerobic exercise if it is deemed safe for your condition by your cardiologist.
Aerobic exercise entails activities that incorporate the large muscles of your body and are continuous and rhythmic in nature (i.e., walking, bike riding, swimming).
You’ll want to customise the frequency, intensity, time (duration), and type of exercise to suit your individual condition and personal preferences.
Exercise frequency
You can perform aerobic exercise anywhere from three to seven (3 – 7) days per week depending on your level of conditioning and exercise tolerance.
If you’re already physically active, you may be able to tolerate more days per week, but if you’re an exercise newbie, then it’s probably better to start off with fewer days per week and work up from there as you adapt.
Exercise intensity
Under normal circumstances (without a-fib), you can use percentages of max heart rate as a gauge of exercise intensity.
But with a-fib, it’s not so straight forward given the variability of the ventricular heart rate.
Commonly prescribed medications such as digoxin, calcium-channel blockers, diltiazem, or beta-blockers alter your heart rate response and therefore may render useless heart rate calculations.
Even so, it’s still not a bad idea to keep tabs on your exercise heart rate so you know what your individual response is under the effects of your medication regime.
If you have a hard time finding your pulse, consider getting yourself a heart rate monitor or a Fitbit (which also tracks your non-exercise movement habits).
I also recommend using what’s known as Borg’s 6 – 20 rating of perceived exertion (RPE) scale.
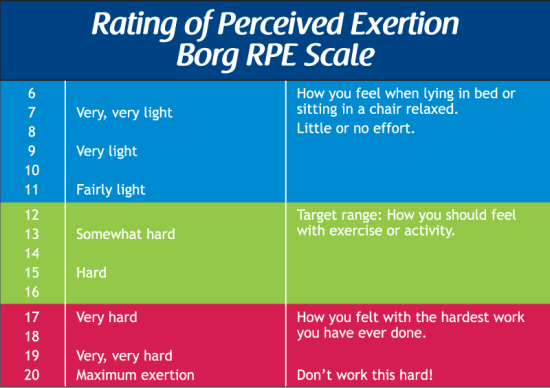
In brief, RPE is a way to use your subjective opinion of how hard exercise is so you can tailor your efforts accordingly.
In cardiac rehab, we recommend beginning with an RPE of “light to moderate” (11 – 12 on the RPE scale). If this feels manageable, then you can graduate to “somewhat hard to hard” (13-14).
Another alternative is what’s known as the “talk test.”
If you can have a conversation with an exercise buddy, then the intensity should be approximately “moderate.”
If you’re huffing and puffing a bit more but can still maintain the conversation, then this would be “somewhat hard.”
Anything higher than that to where you genuinely cannot maintain the conversation is likely too hard.
Exercise duration
If you’re new to exercise or very deconditioned after a difficult hospital stay, I would recommend starting off with short, incremental bouts of exercise.
Begin with 5-10 minute intervals of low to moderate intensity activity.
Perform multiple intervals throughout the day in order to accumulate 30+ minutes per day.
Progress to longer intervals but slowly reduce the number of times per day you do them.
Perform longer bouts until you’ve made it to 45 minutes of continuous activity (as tolerated).
Sample exercise regimen for atrial fibrillation
If you’re feeling overwhelmed fearful and have been physically inactive since your diagnosis, this sample graduated exercise plan can help you transition back to your previously levels of activity.
The aim is to perform more exercise bouts for shorter duration early on and progress to longer durations for fewer times per day.
| Week | Minutes | Times per Day |
|---|---|---|
| 1 | 3-5 | 6-8 |
| 2 | 5-10 | 4-5 |
| 3 | 10-15 | 3-4 |
| 4 | 15-20 | 3 |
| 5 | 25-30 | 2 |
| 6 | 30-45 | 2 |
| 7 | 60 | 1 |
Weight training with atrial fibrillation
I recommend you speak to your doctor before participating in resistance training exercise to ensure there are no medical reasons (aside from a-fib) that would preclude you from lifting weights.
Generally lighter weights are well-tolerated, but higher intensities might pose a risk in those with underlying high blood pressure, known coronary artery disease (blockages in arteries), ventricular arrhythmias, or congestive heart failure.
If you can perform lifting exercises under the watchful eye of a clinical exercise physiologist who can monitor your heart rate and blood pressure responses, then you can experiment to find the right weight, reps, and sets appropriate for you.
Medications and their effects on exercise
There are a few medications that are frequently prescribed for people with a-fib. The main goals are to control or maintain a safe cardiac rhythm and minimise the risk of clot formation (which can lead to stroke).
Common medications include:
Channel blocker
Channel blocking and anti-arrhythmic medications act on your calcium, sodium, or potassium channels and serve to keep your rhythm under control.
They slow down your heart rate and reduce the strength of the muscle cells’ contractions.
Examples include Diltiazem and Verapamil (among others).
Sodium channel blockers slow down your heart’s ability to conduct electricity.
Examples of these medications include Quinidine, Propafenone, and Flecainide.
Potassium channel blockers slow down the electrical signals that contribute to atrial fibrillation and include common meds such as Sotalol and Amiodarone.
Beta-blocking meds can also be prescribed and these act by slowing down your heart rate by blocking the effects of epinephrine.
The end result is a lower heart rate and blood pressure.
Blood thinners
Blood thinners are important because they minimise your risk of clot formation and, consequently, a stroke or heart attack.
Common examples of this include Warfarin, aspirin, Apixaban, or Rivaroxaban.
Interaction of medications, exercise, and atrial fibrillation
If you are prescribed medications, then you may need to alter your exercise prescription.
First, your exercise heart rate will not climb to the same levels it did before you were taking the medications.
So if you use a “heart rate training range” then the calculations are probably not going to be accurate.
In this case, use the Borg Rating of Perceived Exertion (RPE) scale.
Try to find an intensity that is consistent with an effort level of around 12 to 13 (moderate to somewhat hard).
Second, you may find that your blood pressure will not climb as high as usual and this can leave you feeling a bit more fatigued than usual.
If so, remember to give yourself time to adjust to the medications and recognise you may need to readjust your workloads.
You can slowly work back up to the higher workloads as you readjust to the meds.
Third, your blood thinners, by very nature, increase your risk of bleeding, both internally and externally.
You may notice easy bruising if you bump your arm or leg against something.
It’s generally advisable to avoid contact sports since this can increase your risk of internal bleeding.
Work with your doctor to find the medications that get the job done but do not completely bog you out with strong side effects.
This might take a little bit of trial and error, but explain your interest in exercising and ask which ones will be most complementary to getting active again.
Take home message
Atrial fibrillation can be a scary condition, but your best weapon is a thorough evaluation and diagnosis and education on how best to manage it.
I have worked with countless patients with atrial fibrillation and most go on to live completely normal and uneventful lives (no news is good news, right?).
In nearly all cases, they were able to exercise quite safely provided their condition was medically managed and well-controlled.
May last wearing of a heart monitor for a two week period did show a 14 min period which my cardiologist called atrial flutter. This has been occurring on ond off for about 5 to 6 years. Doctor has me on topril, full asprin, and Lisinipril for bp. He wants me now on coumidin. No check of my blood thinning rate has ever been done. Is this an important factor in deciding what blood thinner to take? Thank you,
Hi Ralph,
Without being fully aware of your entire clinical picture, I couldn’t reliably answer your question. However, you should bring this to the attention of your doctor and ask him if he’s going to check your INR (http://en.wikipedia.org/wiki/Prothrombin_time). Or is there any reason to NOT check it? Always remember you have to advocate for yourself in the medical world. Kind regards
Thank you for your positive comments regarding exercise with Afib. Although I had my acute MI over five years ago now – I have only recently been diagnosed with Afib. For over a year I have been riding a stationary bike for 30 min and walking 30 min on a daily basis. Since the onset of Afib I have cut back because I often don’t feel well in the mornings. But once I do feel well enough it’s good to know I can start exercising again.
I don’t have health insurance (or a doctor), I’m a 50 year old male athlete and coach, about 11% body fat and run 28 miles a week. Mom had AF and I feel something happening from time to time. It usually lasts for a few seconds. If I feel it while exercising, my performance is barely affected. I am moving to Italy in a few months and will have medical coverage there. For now, I’m on a self prescribed 81mg aspirin therapy. Can my rigorous exercise regiment hurt me?
Hi Alfonso,
There has been talk about a link between endurance exercise and atrial fibrillation, but I wouldn’t go as far as saying that this is a foregone conclusion for everyone. Link here: https://www.sciencedaily.com/releases/2009/06/090621143221.htm While I have not investigated the nuances of the exercise to AFib link, when you consider the negative health effects of doing nothing, I’d rather see someone exercising with a very miniscule risk of an arrhythmia than die of obesity-related illnesses. You also have to consider just HOW MUCH training might cause cardiac arrythmias, and I would bet this threshold is different from person to person.
You mention having a little flutter in your chest once in a while. You should know that the occasional “skipped beat” in the form of a premature ventricular contraction (PVC) or premature atrial contraction (PAC) are no big deal and are seldom “treated” since they are not sustained. However, if you start getting multiple runs of them that do not spontaneously resolve in short time and you are symptomatic, then clearly you’d be well advised to see someone (no matter what the cost).
While I cannot give you any specific medical advice, I think a wise and prudent course of action would be to stop worrying, get over to Italy where you’ll have health insurance, and then get in to see a cardiac specialist. They can put you on a holter monitor on for a couple days and get a look at your ticker throughout the day and when you’re asleep.
Hope this helps.
Cheers,
Bill
Thank you Bill,
That really helped. Every episode I have spontaneously resolves itself within seconds and I also experience the skipped beat occasionally, with little or no loss of performance. I feel great physically and a lot better mentally with your comment. I will seek a professional as soon as I arrive in Italy. Grazie mille! (Thank you very much!)
Good onya, Alfonso. Likely nothing to worry about, but again it’s VERY wise to get a cardiologist to do a full check over and see how you go. Holter monitor may reveal a bit more, especially if you’re able to wear it before, during, and after exercise to see how your rhythm responds at different phases of exercise. See how you go and keep me posted. Best wishes, Bill
I am 29 (female) and have had two episodes of A-fib within a year of each other. Both times I was hospitalized and it took between 8 to 12 hours to get me back into NSR. Now my EP has me taking 50 mg twice a day of flecaniade and a baby asprin. However, I am nervous about the long term effects of the medication. I would rather not be on it. Sometimes I get dizzy and I still have feelings of skipped beats and a twitch in my heart. I also have shortness of breath during meals. I have been to three doctors and have had countless monitors. Everyone keeps saying that this won’t kill me. Would it be benificial for me to continue the meds. Also, I want to have more children and that scares me to if I’m taking the meds while I get pregnant.
Hi Heather,
Thanks for your comment. As with my response to Susan above, it is important that you discuss these matters with your cardiologist and perhaps explore other options. At this point, because your A-Fib is a bit transient, I can’t see why they’d do anything more invasive like an ablation. You are still very young and, I would agree, in this case it seems like more of a nuisance than anything imminently life-threatening. Perhaps it would be helpful to discuss your meds again with your doctor and explore other options. You also have to weigh out risks versus benefits. That is, the risks of taking the medications versus not taking them (i.e., uncontrolled A-Fib). I would be hesitant to take advice from anyone who is not intimately familiar with your condition (i.e., your cardiologist). If not satisfied, it may be an option to look for another cardiologist, but I would advise against anything too drastic. Keep me posted on how you get on with this. Send an update when able. Kind regards, Bill
Hi there. I have a strong family history of A-Fib. I am 54 and I have normal B/P and cholesterol. I eat a very heart healthy diet with no sugar or saturated fats at all. I have been having atrial fib. It lasts about 15 minutes. It does resolve spontaneously. I was exercising about an hour a day. My symptoms include SOB, mild chest pain, dizziness and weakness. I usually feel like I am going to pass out if the Atrial Fib lasts more than a couple of minutes. I am on a monitor. I really want some advice, but I’ve only been to the ER. I haven’t seen a cardiologist yet. Please help.
Hi Susan,
thanks for your comment. I would strongly suggest that you make an appointment asap to see a cardiologist. Of the different arrhythmias you could have, AFib is not the end of the world. In most cases it can be well managed and not present too much of a thorn in your side. I would like to be able to give you advice, but this is beyond my scope of practice as an exercise physiologist. The only person that should be giving you advice is the cardiologist that runs tests on you and has a full understanding of your condition. Perhaps not the answer you were looking for, but I think it’s the most safe, reasonable, and prudent advice you could be given. Keep me posted and let me know how you go with this. Kind regards, Bill
I have read others people’s comments about their a-fib. Mine however is chronic. My heart fibrillates daily. Even though i take meds for it. It doesn’t do much good. Medicines I’ve taken will work for a few weeks then quit working. But I desperately want to exercise and lose weight. I’ve already lost a little but only due to dieting. Any advice?
Thanks for your comment Velicia. I can certainly understand your frustration having worked with a lot of people with chronic AFib. You would need to speak with your electrophysiologist first, but perhaps it catheter ablation may be an option for you? I did a quick google search and came up with this link: http://www.news-medical.net/news/2006/03/07/16418.aspx which may provide a little more information. No guarantees, but if this is affecting your quality of life (and it seems like it is), then it may be worth exploring this option. Thanks again for your comment. Keep us posted on your progress. Warm regards, Bill
Thank you for writing this article. I’m a 26 year old female who has a hx of palpitations and tachy. I recently completed a 2 week loop event recorder in which I had one reading stating “sinus tach vs atrial flutter block @ 150 bpm” I have had a lot of anxiety about this result and my doctor decided to send me for an EPS in the near future. Thank you for writing such an amazing and positive article. In the meanwhile, my doctor prescribed a low dosage calcium channel blocker to manage my symptoms however, being a relatively healthy young female my bp keeps on dropping too low with this medication. Thank you for making me feel a bit better about the possibility of having atrial flutter.
Thanks for your comment Marie. Agreed, this is a scary thing to have happen to you, but sometimes the fear can be worse than the condition! Better the devil you know than the one you don’t know. It will take a bit of adjustment but hang in there and just make sure you’re on top of your condition at all times. If you have symptoms, then be sure to get them checked out asap. I’ve worked with some complicated patients in the past (people waiting for heart transplants etc) and you’d be amazed at how durable the heart really is. Stay positive!!
The old saying of “when you hit 40 your body starts falling apart” came in spades for me. In 2011, I had a bout with A-fib and had a cardioversion. Later in the year I was diagnosed with Multiple Sclerosis. I have elminated alcohol, cut back on caffeine and have lost 60 lbs. and have been very active. However, just recently while on a week-long camping trip that involved rigorous exercise, I fell back into A-fib. Thankfully, I took Metropralol and Propefenone and the A-fib stopped in a matter of hours. I am discouraged because I thought I had eliminated the triggers and now I fear that I will be unable to exercise like I’ve been doing. I was in training for a major endurance competition next year and fear that I will no longer be able to participate. How can I exercise safely but effectively? I know, loaded question, but I’m feeling really down about this. Thank you.
Hi Aaron, thank you for sharing your concerns. While I am unable to give specific exercise advice for legal reasons, your best bet is to discuss your concerns with your cardiologist and explore options for getting you stabilized and on a path towards your endurance event. I know it may not be the answer you were looking for, but rest assured, I have seen a lot of people with AFib come through the clinic and they have gone on to live robust lives just the same. Keep up a positive attitude!
I’am 71 yrs old and have a-fib for approx. 6 yrs, I work out
3 times a week with weight machines. I work out my back ,
chest and shoulders on these days, I also warm up on the bike. My bp is normal same with my cholesterol and my weight
is 180 ,my height is 6′. I’am on coumadin and been taking it for 6 yrs, I would like to get on a cayenne regiment is
this wise, I have no symptoms.
Hi Frank, Thanks for your comment. For legal reasons, I am unable to give specific recommendations. Your best bet is to discuss this with your general practitioner or specialist (cardiologist) and see if there are any reasons why this might (or might not) pose a problem. Best wishes!
I recently developed Atrial Fibrillation during the recent extreme heat wave that we had in Italy this August 2012. I was/am on blood pressure pills. One day, I felt exhausted, tired, and after finally making it home I measured my blood pressure 86/56 where as it is normally about 140/80. I was told that doctors should warm us to at least decrease the pills or stop entirely during the extreme heats days. too late, I almost immediately started to get Atrial Fibrillation on and off. I started taking a herbal of Omega 3 and Omega 6, and it “seems”, I no longer get them except slight at times. I did have a complete text, exams, charts after carrying a holter for 2 days and my Cardiologist has now subscribed SOTALEX 80 mg but to take 1/4 tablet as an initial test to see if I get dizzy. If so, stop. I am feeling a lot better even before starting any pills. I still take the blood pressure pills however. I am mainly worried that if I do take that SOTALEX pill and start the cure or therapy, that I will never be able to stop them if I feel better. IOW, do I need to take the pill for something I don’t feel bad in Atrial Fibrillation or at least had but now is gone? Worried before I start a cure fro something I no longer have, Atrial Fibrillation. My wife insists I take those pills because of course my family worries that I could suddenly have a heart attack or stroke. Help please. Thank you…
Hello – I am a 37 year old male and I have been experiencing events similar to those described here for about 5 years. Episodes and can be intermittent for several hours or several days. I have a history of high blood pressure and take Toprol as directed. I have talked with my regular doctor as well as a cardiologist in which I wore the holter monitor, stress test, EKG’s and ultrasound of heart. Doctor can he can find no abnormalities. But many of the symptoms described of A fib and arrhythmia are very similar to what I experience. It’s a very scary time when I have these episodes. Is there anything I can do to better describe my conditions that would result in the doctor picking up on this?
Hi Anthony,
Thanks for your comment. It sounds like you’re describing it fairly well, though sometimes what you feel and what might turn up on an ECG are not the same thing. I cannot give you specific advice, but it may be worthwhile speaking with your cardiologist again and seeing if they can do a repeat holter monitor on you. However, based on your previous tests, it is good news that the tests which were conducted did not find anything too sinister. Let us know how you get on with your follow up. Cheers, Bill
Hi, I started getting AF when I was pregnant with my 3rd child 7 years ago, my resting heart rate went up to 120bpm, my weight was the highest ever at 15 stone, I was always 10 stone before.I had one bad episode of AF that took 26 hrs to bring down it peaked at 240bpm. I then had ablation and was told mine was a different type as I had 2 natural pacemakers trying to work my heart ( something along those lines) after ablation (maze something) was done my heart wouldn’t come out of AF again until next morning when I was taken down to have my heart stopped then restarted, I think the fear of having it stopped jolted my heart back to its RHR of 120 again and I didn’t need it done. I still have very short episodes of AF 20 secs max sometimes 2/3 times a day sometimes not for a whole week. My RHR is now around 100bpm. I also have a mild mitral leak.I am going to the gym mon-fri doing 1/1.30 hour on gym equipment and swimming half a mile sometimes weekends to, but my heart keeps setting off the limits on machines as I am getting up to around 200bpm, I can only sustain a 12mph run for about 1 minute and find jogging at 8mph harder to do, I cannot seem to go more than a minute before having to slow down to a walk, it then takes me about 3 minutes to get back to 144bpm at a fast walk of 6.3mph and doesn’t come down to a comfortable 110/120 until I get off treadmill. It doesn’t feel like its my heart affecting my jogging, but I just don’t seem to be able to get past the out of breathe stage.
I am 42 female 14st.8lbs 5’7″ tall and have always been active as in I do endurance horse riding, so though overweight not completely unfit, but am I safe to continue with doing any form of jogging/running? I am obviously wanting to get slimmer and have lost just over 2 stone in 8 months. Will I get fitter and be able to jog longer or is it purely my high heart rate that is stopping me being able to jog, I watch fatter girls than myself jogging for 20 minutes or more and can’t understand how when I am less fat than them I can’t get past a minute or so.I can use ski machines rowers etc and though feeling strenuous can carry on for how ever long I choose comfortably. I am just worried that I might give myself a stroke or something, I don’t take any medication, but was advised to take asprin every day which I don’t as I don’t want to end up with stomach ulcers. I was also told I would have an echocardiogram done every 2 years after the ablation but have never been contacted to do so in the last 7 years. Can I ask to be done or is it because they don’t think I have a risk?
Dear Danielle,
You certainly have a lot to deal with and clearly I can sense in your frustration. One of the most important things to remember when it comes to exercise and any medical condition is to ensure that 1) your condition is medically stable and 2) that you are cleared by your specialist for exercise. If it’s possible to have a supervised stress test performed, then this might provide you with more detailed information regarding safe exercise limits when you’re at the gym. Be advised that I cannot legally give you specific advice for your situation without being fully aware of your entire medical history. I can only speak in general terms and am thus relegated to deferring to the better judgment of your specialist. However, you might also consider looking for a second opinion from another specialist who has a strong exercise/sporting background (i.e, triathlon, etc). They would be more sensitive to your situation.
As for stroke, again, this is another very real risk. It may be worth speaking with your specialist to discuss options, types of aspirin (coated, etc), dosages. Best thing is not to give up on dialogue and get further clarity of every option at your disposal.
As for the echocardiogram, again, this is something worth mentioning to your specialist. People can and do slip through the cracks of the medical system all the time, so I would be a bit more proactive and at least phone them to find out. Bring this to their attention and get to the bottom of it, but never assume anything when it comes to your health. Get answers and you’ll probably sleep a lot better at night.
Keep me posted on how you go after you follow up with your docs.
Kind regards
Bill
I have had irregular heartbeats for many years. MI at age 50. Bypass at 78. Am now 88. I took Amioderone for several years but ceased last year upon advice of my doctor. I exercise regularly on treadmill during which my heart rate will sporadically, suddenly increase to 150 or so and revert to normal within a few seconds. I am told one of my valves is not functioning normally. Wearing out. Underwent a 30 day monitoring, which showed numerous fibs and flutters. Am now taking warfarin. BP is under control. Taking Exforge 5/320. Exercise (treadmill) helps me maintain a positive attitude and I want to continue with my routine. Should I be fearful of the fibs and flutters? Should I just continue confidently with my sensible exercise routine, considering my age et al. Please respond.
Hi Gerald,
You should be aware of runs of afib and aflutter, but I would not advise being fearful. This may prompt a bit of anxiety which might actually provoke their onset. Your age is not really the main factor, as I have worked with people of all ages and have seen some pretty fit, healthy, and strong 96 year olds…even after an MI, surgery, and everything else.
Though I cannot give specific advice for anyone’s condition without being fully aware of the entire medical history, in your case, I would strongly suggest having a more detailed conversation with your cardiologist and discuss the options. It might be worth talking about having a cardiologist-supervised treadmill stress test to determine what exercise intensity sets it off. If you have an exercise physiologist present, they can help you work out the details. It might be helpful to wear a heart rate monitor and track your normal heart rate response and at what point (and at what intensities) your afib is set off. A little bit of trial and error.
Hope this helps. Keep me posted on how you progress. Best wishes to you.
During a recent Nuclear Stress test, at the end of the test (10.5 min @ 4.25 mph and 16% grade) I experienced an SVT. For the past few months leading up to this visit I felt I could feel my heart beat while resting. I wore a monitor for 24hrs after the stress test and the follow visit indicated I had A-fib. For the past ten years I have been an endurance cyclist. During the week I would ride anywhere from 12-40 miles per day and use these trips as training doing intervals and riding where my heart rate was around 130bpm. BTW, I am 67 years old.
Now, I still exercise at least one hour per day at the gym on a recumbent bike or elliptical machine but I sure miss those long rides of 40-100 miles each. My cardiologist has increased my Lipitor to 80 mg every other day and put me on 20mg of Xeralto. I have experienced no side effects from either of them. My blood pressure is excellent 110/62 and my resting heart rate is 58bpm. My question is do you think I could resume riding on the weekends, at least one day, of between 40-100 miles if I ride leisurely instead of maintaining a higher heart rate, say keeping it around 112 bpm?
BTW, after the stress test I checked my riding history and saw that I had registered heart beats per minute over 200bpm on a few occasions using my Polar Heart Monitor. I didn’t pay any attention to them as they were infrequent and I wrote it off to heat and/or a transient signal.
Hi Harry,
Thank you for your comment. I’ll say a few things here. First off, you may be aware that there is suggestive evidence that endurance athletes (which you clearly are) have a higher risk for the development of dysrhythmias.
Second thing is, while I cannot give specific advice to anyone without being familiar with your entire medical history, I can say it appears you are still quite fit and doing much more than most 67 year old men. I would encourage you to speak with your cardiologist about your desire to increase your distances. If you’re well managed then it may be feasible. Thing is, at least NOW you know what you’re dealing with, whereas before you were operating in the dark. And THAT is truly more dangerous than exercising with an arrhythmia and not knowing it! I agree, your polar likely picked up your runs of SVT. I’ve seen this before in clients I’ve worked with, so again, better the devil you know than the one you don’t!
Third, if your cardiologist is not exercise savvy, perhaps consider shopping around and changing to a cardiologist who is an athlete himself and understands the athlete’s mindset. I’m not telling you to just find someone who will tell you what you want to hear, but rather one who is intimately familiar with serious training and understands the point at which both training and cardiac conditions intersect.
Hope this helps!
Kind regards,
Bill
Thanks very much for your quick reply. You more or less have confirmed what my cariologist has indicated to me. I have selected him because of his work and research with local atheletes and the fact that he himself was a marathon runner at one time. I will be sure to confer with him about my desire to ride long distance at least once a week. Thanks again for offering a very helpful website.
Harry C.
My mother has atrial fibrilation for more than a year. She has seen more than 5 doctors who say that the condition is “incurable” and prescribed her medicine prodaxa and bystolic She recently started exercising and I am concerned whether this might be harmful if shes taking blood thinners. Also if she does start feeling better from the exercise can she stop taking these harmful medications. I am concerned because the doctors do not say anything about what she can do to relieve this or help the condition they just say that it prevents from stroke or heart attack? will it be safe for her to exercise with the medicine
Hi Lana,
Thank you for leaving a comment. There are a few things to consider here and I’ll spell them out below:
1) Even if afib is incurable, this condition is not a death sentence.
2) There is no harm in her taking blood thinners unless she has any specific conditions which might be worsened by these. Any diligent doctor would have screened her to make sure it was an appropriate treatment. If she was to (god forbid) fall and bang her head, then blood thinners would certainly not help the situation much (at which time she would need immediate medical attention).
3) The meds do prevent clot formation, one of the risks in people with AFib. She is more at risk if she doesn’t take the blood thinners.
4) If she starts feeling better from the exercise, the only one who can take her off the meds is her doctor. If you come across someone online who says it’s ok for her to stop taking the meds (without being familiar with your mother’s medical condition), then they are practicing medicine without a license.
5) As for if she can exercise while taking the meds, I’ll say this. I have worked with a LOT of patients who have had no problem with exercise while taking blood thinning medications. However, as I stressed above, you will need to make sure your mother gets clearance from her doctor to exercise. Once this is in order, I would suggest contacting a clinical exercise physiologist in your area. Your local hospital may have some names and phone numbers for you.
Best wishes,
Bill
I’ve been in Afib for about two years now. I have a wonderful electro cardiologist and he prescribed Pradaxa. I’ve adapted well to the med and exercise 6 times a week. The only drawback is I don’t do sprints as I used to. I swim 4 times a week (former Master’s swimmer ) and run 2 times a week. I have a normal heart but would love to sprint again as I used to . It was one of my favorite things to do in workouts. Now I swm LSD (long slower distance) and jog rather than push it. My cardiologist said that I am an excellent candidate for a catheter ablation. My hesitation is only that when I questioned him about the permanence of the procedure he admitted that I’d probably have to repeat the CA in a few years. So I thought: “Why bother”. Though I’d love to compete again in Master’s Swim meets. I’m almost 70 and I’d be at the top of my class if I could get my sprint ability back.
Do you think its worth it or do you think the risk is too great or the “benefit” is too minimal. Tell all those Afibers that with Pradaxa I’ve had no problem exercising consistently “IF” a bit slower.
Thanks, Joseph
Hi Joseph,
Thank you for your comment. I do not give any specific advice on this site other than that which is within my particular scope of practice (clinical exercise physiology). Based on my work in cardiac rehab, I encourage people to discuss these types of questions with their cardiologists and weight out the risks versus benefits. If you’re able to manage it effectively with a medication, then you’ll have to weigh out if a surgical risk is worth it. If the meds are not doing the trick and it’s cutting into your quality of life, then perhaps the risk is something you’d be willing to take. I wish I could give you more info, but without being a cardiologist and knowing your entire medical history, it would be illegal for me to give you specific advice. Keep me posted on your decision.
Kind regards
Bill
For several years I have had episodes of atrrial flutter with no impact other than a minor loss of energy. Recently I had a TIA which was attributed to the AF. I am 59 in good health 8 kg over weight, with no cardiac disease, low cholesterol, clean arteries no alcohol, no tobacco etc.me ECG was clean. my cardiologist has whittled the cause of AF to sleep apnea as it always seem to onset overnight and disappears during the day or again overnightas well as the fact that I snore. With all that preamble. I have noticed since I have commenced taking brisk walks, the AF disappears under heart load. Eg 90+ bpm. My normal resting bpm is about 60. Does this suggest that the AF has something to do with oxygenation and may therefore be connected to sleep apnea as suggested.
Hi Mitch,
Thanks for your comment. There does appear to be an association between sleep apnea and atrial fibrillation though the precise mechanism behind the relationship is still debatable. I’d say it is plausible that hypoxia (low oxygen) might play a role, but when we look at an association between conditions, this does not always indicate a cause and effect relationship in one direction (i.e., does sleep apnea cause AF, or does AF cause sleep apnea). Let me know how it goes for you. Kind regards
What sleep medicine is ok with A-Fib?
Hi Bruce, only your doctor can answer that question since he/she is familiar with your entire medical history.
I am 58 yo and an ED physician with paroxysmal AFib. I have been physically active all my life and am otherwise healthy with a structurally normal heart. I probably have had minor short-lived episodes since my early 30’s but in the last year and a half have had 3 prolonged episodes which reverted with propafenone. I still go to the gym and do crossfit style workouts. I know the studies have focused on risks with intense prolonged exercise regimens such as long distance running and cycling. Are there any studies looking at longterm risks for individuals with PAF and short, high intensity workout programs? ( The three prolonged AF episodes occurred in the context of high intensity workouts and limited sleep) I now use a heart rate monitor and keep my heart rate below 160. Thanks.
Hi Jonathan, Thank you very much for your question. I think you’ve identified a gap in the afib medical literature. Likewise, most of what I’ve seen deals specifically with endurance type exercise and it’s association with atrial fibrillation. But paroxysmal afib and high intensity exercise is still a bit nebulous in terms of consensus. Having said that, I’ve worked with a number of patients over the years with PAF and found that, independent of the exercise type, it was important to identify the triggers that set off the afib. In your case, you point out that it happened to you a few times with high intensity exercise and limited sleep. When you get adequate sleep, do you find that it doesn’t occur? And you mention keeping your heart rate at 160 or less. Have you found that your afib was set off at higher heart rates? I’m a fan of continuous telemetry monitoring during exercise and have found that doing a bit of trial and error can help identify the threshold at which the afib is set off. I had a client who was completely normal in every way except that her afib was exercise induced when she was on steep inclines at about 160 bpm. When she stopped doing steep inclines and kept her heart rate under the 160 mark, she noted a reduction in afib episodes. Admittedly nothing official or scientific, but it was a temporary management strategy until she had her ablation done. In your case, you sound like a switched on guy and have got your ducks in a row, so I think your strategy of nothing the circumstances which precede runs of PAF would be your best bet for the time being. Obviously if it’s something that becomes more frequent and requires intervention to get back to sinus rhythm, then you’ll explore other options for treatment. But the bottom line regarding research is I don’t think there is much out there beyond the usual endurance exercise/afib research. Kind regards, Bill
Thank you for this article. I’m a 50-year old obese woman with very high blood pressure and a-fib. I had a cardiac arrest 3 years ago (probably caused by a blood clot) and consider myself lucky to be alive. My arteries and cholesterol are fine for the time being and I don’t appear to have any more serious health issues.
I’ve enrolled in a slimming class and am determined to improve my overall health. I’ve been told that there’s no reason I can’t exercise normally, but am at a bit of a loss as to what to do. Walking upstairs or uphill is a chore that leaves me breathless, and I have back and knee pain, probably weight related.
I used to be very active when I was younger, and can walk around quite well as long as the ground is level! 🙂
Should I try more exercise now, or wait until I’ve lost a bit more weight? My cardiologist wasn’t really much help in this regard. 🙁
Dear Angela,
Thank you very much for taking the time to leave a comment. You’ve certainly had a few health scares, but I’m glad that you have arrived at a point where you are now ready to get back on track and get healthy again. Provided there are no pressing medical limitations that would preclude you from doing exercise (and you have clearance to do so from your doc), then exercise, even at low levels just to get started, is one of the best things you can do for yourself.
First off, being overweight can really crank up the perceived intensity on movements like walking up stairs and up hills. While starting off, I would recommend two things: 1) try to focus on walking on flat/level ground for a while in order to simply build up your fitness foundation; and 2) when you take the stairs or walk up hills, just be sure to do what you can do, take a rest/breather as necessary, and then continue when ready. What will happen over time is that, independent of how much weight you lose, your body will adapt and develop a training effect so that stairs and hills are no longer the struggle they once were.
Your comment about knee pain is not uncharted territory and, in fact, is quite common in people who are carrying a bit of extra body weight. BUT, the good news is that as long as you are gradually easing into your exercise and slowly building up your foundation, you will find that you can tolerate more and more exercise without as much knee pain. Plus as you start to shed the body weight, the absolute gravitational load on your body will be less and you will probably have less knee pain (a double whammy benefit!).
I have outlined some guidelines for exercise in my angioplasty and exercise article. Have a look at these since they are general recommendations which can apply to your situation: https://drbillsukala.com/exercise-after-angioplasty-stent/
Hope this helps you get moving in the right direction. Keep on going!
Warm regards,
Bill
I am 65 years old. I had a mitral valve correction operation in 1995 after suffering from MR since childhood. As a result I have an enlarged LA (5.4 cm) and AFib. I feel OK and does Pilates and uphill walking daily. I asked my cardiologist about resistance training in the gym. He told me to avoid it. From my experience a repetitive exercise like walking does not reduce fat % in your body as effectively as resistance exercise. What do you think I should do to in order to build up muscle and reduce fat % in my body.
Hi Yuval,
Walking does help you reduce body fat, but like with any exercise, you have to remember to help it along with healthy eating as well. I would discuss your condition with your doctor and perhaps find a qualified clinical exercise physiologist to help you find some resistance exercises that may be appropriate for your particular situation. You might not be able to lift heavy weights, but some moderate level resistance training my provide some benefit if you are deemed medically stable and are working with a clinical exercise physiologist with cardiac rehabilitation knowledge and experience. I hope this helps.
Kind regards,
Bill
I am a 75 year old lady diagnosis a year ago with PAF. I take Bisoprolol 2.5 mg and Rivaroxaban 20 mg. I used to do a lot of hard exercise. I am nervous about riding my bike. My husband keeps pushing me to ride my bike. He thinks that maybe i should be on a higher beterblocker ,as that might help my PAF.
Hi Joyce,
You can exercise safely with atrial fibrillation provided that:
1) you are medically stable; and
2) you have received clearance from your cardiologist to exercise.
If you have a cardiac rehabilitation program near where you live, I would also recommend that as a way to help guide you safely back to exercise. I am certainly understanding of your nervousness, but as long as you bear in mind the safety considerations I’ve mentioned in my article, you can significantly minimise your risk.
Kind regards,
Bill
I am a 66 year old male who has been a recreational jogger for 28 years. During a routine EKG I was diagnosed with AFIB. I underwent a nuclear stress test and echocardiogram as well as carotid and leg ultrasounds. My doctor says they all showed no blockages. He recommended a return to my exercise routine of 4-5 times a week on the treadmill for 40 minutes which produced a 3 mile jog. During the stress test I was unable to get on the treadmill because I was in AFIB by just standing. They induced the heart rate to increase with drugs and my heart rate spiked above 170. It gradually came down over the next 15 minutes. Previously my resting heart rate was 53 and my max workout rate was 130. Today during a 30 minute walk my heart rate started at about 120, spiking to 165 (max) with rapid fluctuations. The “normal” rate during this exercise rose from the 120 to about 155. My new normal resting rate is about 80. I am taking metoprolol, amlodipine and lisinopril (and have been for years). I have been taking Eliquis for the last 6 weeks. Should I be concerned about exercising at this level of heart rate given my theoretical 100% rate is 154?
Hi Thomas,
Thanks for your comment. When it comes to your theoretical heart rate, remember that this is just a prediction equation of 220 minus your age. However, hearts can be funny organs sometimes and there are people who’s ACTUAL measured max heart rate is higher or lower than their age-predicted max heart rate. It can be used as a rough guide, but it’s not the end-all be-all.
The big question here is whether or not you’re symptomatic. Are you experiencing symptoms when your heart rate jumps up to 155 (or 165 at times)? I would strongly suggest that you speak to your electrophysiologist (cardiologist) and/or the practice nurse at the cardiologist’s office. Let them know what’s going on because if your heart is acting “out of character,” then perhaps this could require further workup and evaluation by your doc. Your medical management team might also wish to reevaluate your current medications and respective dosages.
Talk to your doc and then feel free to leave a comment again. It is beneficial for other readers with AFib to learn from your experience.
Kind regards
Hi am 48 had st jude valve tissue MVR surgery 5yrs ago cause of history of rhematic ..but my afib didn’t go away.. along wit that my bp spikes up suddenly diastolic 110.. 120 top # 177…am on warfarin am so scared at times why ..and pls help
Hi Vashti,
I’m sorry to hear you’re still having trouble with your atrial fibrillation and blood pressure. I cannot give any specific advice over the internet, but I would strongly recommend that you discuss these matters with your cardiologist who will be most familiar with your complete medical history. It will be important for them to evaluate all your medications and dosages to ensure the best outcomes for your arrhythmias and high blood pressure. If you are feeling very anxious, then it may also be a smart idea to speak to a health psychologist in your area who can help you better manage the thoughts going through your mind. Sometimes, if you’re feeling anxious, then this can have an effect on your blood pressure and heart rhythm. A bit of mindfulness and meditation may also help you feel more calm on the inside. But the first stop for you should be your cardiologist to get the best available information relative to your medical history. Hope this helps. Kind regards, Bill
Cardiologist had me on Bisoprolol…for a year, kept upping the dosages as my last holter monitor showed me with an average HR in the 90’s. Eventually was taking 10mg a day. Since June I’ve been walking almost daily – averaging over 125km/month the past 3 months. But during that time my weight kept increasing, I gained 30lbs and hit 299lbs. Due to developing Tinnitus (an apparently rare side effect) I went off the medication. In 2 weeks with no other changes I dropped 20lbs. Then I read that weight loss is yet another side effect of Beta Blockers. So in summary, people with Afib get put on these drugs, their weight goes up, putting more strain on their heart and the doctors response is to simply increase the dosage making the problem even worse.
Sadly I was hoping exercise and staying away from caffeine, alcohol etc. would be enough to keep my rate manageable, but it slowly but surely is creeping up again. Now I notice after 30 mins on the elliptical my heart rate will shoot up to 180 and stay there for over an hour. I’m worried I’m going to end up hospitalized like I almost was last year when I had a pulmonary edema, found out my heart was enlarged, ejection fraction low, heart at 30% of normal function etc. – which is when I went on the drug (EF improved, functionality almost back to normal). But I simply can’t go back to gaining weight again, and eating say 1000 calories a day and being hungry all the time is not the solution either.
Advice?
Hi James,
While I can’t give any specific advice over the internet, here are some things that I would suggest bringing up in a conversation with your cardiologist.
1) If your heart rate is getting up to a sustained 180 bpm, it would be good to know if you are in sinus rhythm or if you’re in atrial fibrillation. If it’s the latter, then it would make sense that you have a higher heart rate. The other question is whether or not you are symptomatic. Are you feeling dizzy, light-headed, or short of breath? Perhaps ask your doc if it’s appropriate to do a treadmill stress test with full 12-lead electrocardiogram. This might inform the situation a bit more to help determine the best way forward. Also ask if an ablation may be appropriate for you.
2) You mentioned your ejection fraction was compromised. Find out what it is now and how close it is to normal (i.e., around 55% or higher). If it’s relatively stable and isn’t going anywhere, then this may not play into the picture of how much exercise you can do. Still worth monitoring though.
3) I would strongly recommend getting a referral to a clinical dietitian who has the knowledge, understanding, and experience to work with people who’ve had some medical issues. Don’t go to some wacknut self-proclaimed “nutritionist” who did an online course. It’s the same as asking your local mechanic or insurance salesman for nutrition advice (sorry, I had to include that). There is a sh*tload of bad information out there on social media and the internet in general, so I would strongly recommend discussing your diet with a properly qualified nutrition professional. Looking at your IP address, you appear to be located in Alberta. Here are some links to put you on the right path:
http://www.collegeofdietitians.ab.ca
https://www.albertahealthservices.ca/info/Page15808.aspx
Hope this helps put you on the right path. Feel free to stop back and leave another comment.
Kind regards,
Bill
hi
i am 72 and have had AF for some years now and i am on Flecainide acetate 100 mg twice a day. I have continued to exercise regularly cycling ( 3 times a week a total of around 200 km a week) and swim three times about 4km in total. i wear a heart monitor when I cycle – and would experience AF maybe 1-2 every 6 months when cycling. Lasts for few minutes to 30 minutes. If I didn’t have the heart monitor I would not know I had AF.
my big bug bear is that my maximum heart rate varies – sometimes a maximum of 116 and other times 136> I time myself over the same section of a climb – with a maximum of 116 it takes around 9 minutes, when I can get to 136 only about 8 minutes. There is nothing I can do to increase the maximum – it is what it is on the day. I did a stress echo on a treadmill the other day and could only get to 130 bpm after 12 minutes.
Is there anything I can do to have a consistent high maximum heart rate ie around 135. A max of only 116 significantly affects my cycling. Maybe reduce the dosage. Cardiologist didn’t have any explanation why my max varies – and on the day there is nothing I can do to increase it – it is what it is.
Thanks
Hi David,
Atrial fibrillation by its very nature can fluctuate quite a bit and I can certainly appreciate your frustration. You sound like an active guy, so it can be a real kick in the nuts when you can’t seem to get into a good groove with your training heart rate. It’s hard to say exactly what’s going on, but perhaps it may be worth your while to have another talk with your doc about your meds and see if that might be playing a role in this. But variable heart rate aside, sometimes it’s better the devil you know than the one you don’t know. If your atrial fibrillation was undiagnosed, then that would be far worse. Feel free to stop back and leave another comment after you meet with your doc. It’s always useful for others to read your story and perhaps glean some pearls of wisdom (and/or inspiration). Kind regards, Bill
Dr. ;
Good stuff here, so lets go with this. In july, 2018 I was surprised to note at my Cardiologist check up- “you’re in afib”. So, originally it was his path to put me on baby aspirin. Later in August he calls me and says he has reconsidered and wants me to see EP in the clinic he works in. So Dr Yunus sees me in late August 2018, and says given the circumstances of my constant Arrhythmia he schedules a cath ablation in Sept 2018. I go through the procedure and am placed on blood thinners previous to this back to original visit with EP. The ablation was not successful, unfortunately. This past week in late Dec, I went back to visit after the 3 month scarring process to learn he wants now to put more meds into my system, flecainide and metropropol. Seems my condition is more constant than occasional.
I’m a long time athlete, work out 4-5x week for 1.5 hours. Combining cardio and lifting. Skiing, cycling, and running. This new routine of drugs scares me, I don’t feel like myself. The doctor told me no lifting, puts stress on atrium. Indicated that holding your breath causes that stress. I’m early into this situation- am 61 years of age. 6’1′” 185lbs. Not sure what other steps I need to take in the near term. Just gave up coffee completely this week. Am planning on trimming 10 lbs off my frame. Any other thoughts on my recent acquisition of this situation I’m facing. I have to work out, – but am super bummed about my condition and inability to continue on the path I’m used to after 40 years of my habit of physical activity.
Hi John,
I can certainly feel your frustration. The hardest thing is going from being really active to being told that you can’t push yourself. AFib is one of those tricky and unpredictable things too that can really throw a damper on things. I would strongly suggest talking to your doc about a referral to a hospital-based cardiac rehab program. They’ll be able to help you with your exercise and perhaps put you on telemetry to monitor your rhythm while you exercise. More importantly, if anything should happen, you’ll be in the safest place. Plus that, they’ll be abler to give you the best advice relative to your specific medical history. They can interface with your doctor to ensure the best possible care. I have worked with a lot of active people in cardiac rehab and the experience really helped allay their concerns and give them a sense of comfort and control again. As you pointed out, yes, losing weight and cutting out the caffeine will also help you manage it. A-Fib is definitely a wet fish to the face but it doesn’t have to be the end of the road where you just wither away. Better the devil you know than the one you don’t know. There will be some adjustments ahead, but your best bet is to work closely with your medical management team and find ways to maintain your active lifestyle as safely as possible. Kind regards, Bill
Good afternoon Dr.
I am M.S.Patil. I had gone through open heart surgery for severe pulmonary stenosis. It was 110. After operation it is now 25 to 30. I am feeling well. I was told by the doctor that I can do all sort of work exercises. So for first two years, I was determined to do regular exercise. I was feeling well, but last year the problem of missing heart beat was noticed. I posted my problem last year but there was no response from you.
Ok, but my problem is different now. I am doing regular exercise and I am feeling well, but noticed this missing pulse issue. So I consulted my surgeon and he did a Holter Monitor test twice. Then there was a turning point due to stress in my job. I fell into a depression and it took me about six months to come out of this depression. I am now again feeling healthy and going for swimming daily for 45 minutes. My heart rate remains between 60 to 64 beats per minute. The last time when this problem was reported to my surgeon, he suggested to take Orcibest 10mg. Now again I am feeling this missing heart beat. But to feel this missing beat I do not need to feel my pulse. I just feel the skipped beats and feel dizzy for a moment. Also when I take Orcibest 10mg tablet, I notice an increase in heart rate. Please advise what I should do. I feel healthy when I go swimming but this missing pulse appears sometimes.
Hi Maruti,
Thank you for your comment. First, I have gone back and reviewed all your previous comments and can confirm that I responded to each of them. Because I respond to every comment personally, it may take me some time to get around to it because I’m busy with multiple projects. Perhaps you were unable to find my responses at that time. If so my apologies.
As for your current situation where you appear to be having some “skipped beats.” The first thing you need to do is speak with your doctor and confirm what kind of skipped or missing beat you’re dealing with. If you are experiencing premature ventricular contractions (PVCs), these are generally considered NOT harmful. They can potentially become a problem if they become prolonged and you are symptomatic. You mention you are dealing with some dizziness, so this may be a good reason to speak with your doctor and make absolutely sure that you do not have any problems such as atrial fibrillation.
You mention that you are taking Orcibest. One of the side effects of this medication is dizziness and irregular heart beat. It is possible this is the culprit.
Orcibest side effects:
Fast, pounding, or irregular heartbeat
Shakiness in the legs, arms, hands, or feet
Diarrhea
Dizziness and fainting
Headache
Nausea and vomiting
Runny Nose
Cough
Loss of appetite
Bottom line: please see your doctor and discuss this to ensure that it is nothing more serious. If it’s just the medication then you can discuss what to do next with your doc.
I hope this helps.
Kind regards,
Bill
My wife has had 2 different heart procedures in her life. She has had a patch put into repair a whole between heart chambers and they did a maze procedure which then lead to a slower heart rate requiring a pace maker and show she is once again having AF episodes. She has been taking an SSRI for anxiety but I don’t want her to take this forever and have read a recent article you wrote around psilocybin and potential heart valve damage. I am trying to connect with a psychedelic aware cardiologist that can share research on the benefits/dangers of psilocybin usage for heart surgery survivors.
Hi Rodney,
Thanks for taking time to leave a comment/question. So I’m clear, is she looking to take psilocybin instead of an SSRI for her anxiety? The primary concern around psilocybin and cardiac health is related to the heart valve leaflets, but it appears your wife’s heart procedures are related to other things. If you can find a cardiologist who is psychedelic aware, then they can discuss all the details specific to your wife’s conditions. But in general, the risk between psilocybin and heart valve damage appears to be mostly theoretical and has not been demonstrated in any clinical studies. These are extrapolations from other drugs with detrimental effects on heart valves that were also taken daily and in large doses. The amount of psilocybin in a fruiting mushroom body is extremely small and it’s taken infrequently so I don’t think we have enough conclusive evidence to show it would lead to any issues. But the risk is still never zero and it’s for this reason I’d suggest working closely with your doctor for safety.
Kind regards
Bill