If you’ve been diagnosed with hyperinsulinemia, that’s not good news, but it’s also not the end of the world if you take action now to do something about it.
In fact, when I work with clients who have early pre-diabetes symptoms, I explain to them that hyperinsulinemia is like a warning shot across the bow.
What you do next will determine if you progress on to good health or develop full-blown type 2 diabetes.
Therefore, the purpose of this article is to:
- explain what hyperinsulinemia is; and
- the importance of exercise to reduce hyperinsulinemia
What is hyperinsulinemia?
Hyperinsulinemia might look like a long scary word, but when you break it down, its definition comes into focus:
- “hyper-” = high
- “insulin” = insulin
- “-emia” = blood
So as you can see, it’s just a fancy word to describe high levels of insulin in your blood.
Hyperinsulinamia is a sign of an underlying problem controlling your blood sugar, which requires your pancreas to pump out large amounts of insulin to keep your blood sugar levels within a normal range.
As with hyperglycemia (high blood sugar), hyperinsulinemia is not a stand alone “disease,” but is actually a symptom which occurs in the presence of other disease states such as pre-diabetes, diabetes, or polycystic ovarian syndrome in women.
In most cases, hyperinsulinemia is strongly associated with obesity.
Hyperinsulinemia is a risk factor for other diseases
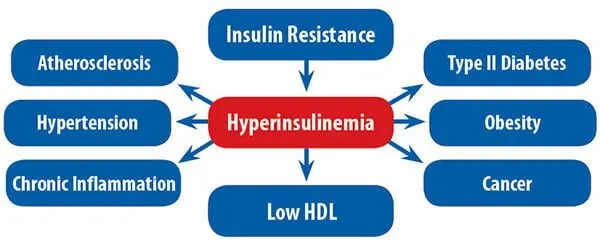
In the image below, you can see that insulin resistance leads to hyperinsulinemia which, if left untreated, can lead to a whole host of other health problems.
What causes hyperinsulinemia?
Before discussing the causes of hyperinsulinemia, it is important to first understand your body’s normal insulin response.
Insulin and glucagon are two hormones that work together to maintain your blood glucose levels within normal limits. Insulin helps bring down blood sugar levels whilst glucagon helps raise blood sugar levels when needed.
For example, when you eat a meal, insulin is secreted to help reduce your blood sugar.
When blood sugar drops too low, glucagon is released to bring it back up to the normal range.
Related Articles
- Is Fruit Sugar Bad For You?
- Carbohysteria: An Open Love Letter to Carbohydrate
- Is Sugar REALLY That Bad For You? An Honest Answer
With hyperinsulinemia, your body’s cells are unable to effectively respond to the effects of insulin – also referred to as “insulin resistance” – thus causing your blood sugar levels to rise beyond normal levels.
Your pancreas tries to compensate for the resulting hyperglycemia (high blood sugar) by pumping out even more insulin to bring down glucose levels, but resistance to the effects of insulin results in persistent hyperinsulinemia.
Pre-diabetes or type 2 diabetes is diagnosed when the body’s compensatory mechanisms can no longer keep pace and blood sugar levels rise and remain persistently elevated.
If your insulin resistance remains unchecked, you may eventually develop type 2 diabetes.
If your diabetes remains uncontrolled, then your pancreas’ beta cells which produce insulin may fatigue and no longer be able to secrete adequate amounts of insulin required to maintain normal blood sugar levels.
At this point, you could be prescribed insulin injections.
What are the signs and symptoms of hyperinsulinemia?
Hyperinsulinemia generally does not cause any outward signs or symptoms.
However, in insulin resistant people, hyperglycemia (high blood sugar) is often present and this may result in symptoms including the following:
- High levels of sugar in the urine
- Frequent urination
- Increased thirst
Treatment of hyperinsulinemia
Treatment of hyperinsulinemia is the same as for pre-diabetes or diabetes.
Lifestyle changes which can help you reduce insulin resistance (i.e., diet and exercise) are strongly recommended, though medication may sometimes be warranted if your situation does not respond well to lifestyle management.
The decision to medicate is often based upon weighing up the potential risks of allowing you to continue with uncontrolled hyperinsulinemia versus the benefits of the medication, which may significantly improve your long-term health outlook.
Effect of exercise on hyperinsulinemia
Exercise is potent medicine for improving overall health, but it is particularly important for people with hyperinsulinemia.
Here’s why.
There are two ways by which blood sugar is taken up into muscle tissue:
- insulin-stimulated glucose uptake; and
- muscle contraction-mediated glucose uptake.
If you have high insulin levels, then that means your body is not responding normally to the effects of insulin and, as a result, your blood sugar levels remain elevated.
On the other hand, muscle contraction does not exclusively require insulin to facilitate sugar uptake into the muscle cells. Exercise is also an insulin-independent pathway for mopping up blood sugar.
If you do regular exercise, then your blood sugar levels drop which has a flow-on effect of signalling the pancreas to turn down insulin production and, consequently, reduces your blood insulin.
When you have hyperinsulinemia, insulin is not an effective signal for blood sugar uptake because the muscle cells get gunked up with fat (intra-muscular triglyceride) which impairs your body’s ability to respond to insulin.
But as you keep exercising on a regular basis and reduce your body fat, you eventually burn off the fat (intra-muscular lipid) gunking up your insulin receptors and your body becomes re-sensitised to the effects of insulin.
Types of exercise for hyperinsulinemia
The best exercise for hyperinsulinemia is the one you’re going to do!
Everyone is looking for the magic exercise, but the reality is that when it comes to conditions like hyperinsulinemia, hyperglycemia, pre-diabetes, or diabetes, any exercise that results in muscle contraction is going to have a positive effect on your condition.
Even standing in one place under gravitational load is better than sitting in one place for an extended period of time.
Aerobic exercise
Aerobic exercise refers to movements which are steady and continuous in nature and incorporate the larger muscles of your body.
Examples of aerobic exercises include long walks or jogs, riding a bike, or swimming laps.
Anaerobic exercise, on the other hand, is usually higher intensity and will leave you feeling fatigued and short of breath.
This type of exercise has merit too, but you should slowly progress to the higher levels from a good aerobic fitness base.
The benefit of aerobic exercise for hyperinsulinemia is that it can be performed by most people no matter the level of obesity or deconditioning.
I’ve worked with massively obese people in my career as an exercise physiologist and can confirm that there are ALWAYS exercise options available no matter what the health limitations.
Weight training
If you don’t like, or find aerobic training to be unfeasible for whatever reason, then weight training can also be a viable option.
Whether it’s lifting iron weights, using resistance training machines, or just pushing around your body weight, these types of movements can have positive and lasting effects on reducing your hyperinsulinemia.
Exercise frequency
Exercise frequency, or how often you exercise, should be dictated by your individual level of conditioning.
If you’re new to exercise, you’ll want to start off conservatively with three days of exercise per week.
As you begin to feel stronger and your tolerance to exercise improves, then I’d suggest increasing this gradually to four to five days per week, and eventually up to daily.
When it comes to high blood sugar levels (and consequently hyperinsulinemia), the more you exercise, the better your blood sugar levels.
The effects of a single (acute) exercise session can have a lasting positive effect on insulin sensitivity for about 48 to 72 hours after the session finished.
This means that even when you’re not exercising, your body is better able to respond to insulin and bring down your blood sugar levels.
Exercise intensity
Exercise intensity refers to how hard the exercise is.
As above, if you’re new to exercise, I suggest easing into it at a low to moderate intensity and then progress upwards from there.
For example, the first two weeks, you might try walking at a leisurely to moderate pace where you can maintain a conversation with your exercise buddy without falling short of breath.
This is what exercise physiologists refer to as the “talk test.”
As your fitness improves, you can gradually increase to include short higher bursts of intensity.
For example, if you’re walking at, say, 5 kilometres/hour (3.1 mph) as your baseline comfortable pace for 30 minutes, then you can intersperse the higher bursts of fast-paced intervals for, say, 2-3 minutes.
You can modify the interval duration up or down depending on how well you tolerate this.
Overall, the trick is to be systematic and progressive in your approach so you can control and monitor your progress.
Exercise duration
Exercise duration refers to how long each session is.
As with the other exercise variables, you’re going to have to go by feel depending on your individual level of conditioning.
If you’re very out of shape, I’d suggest you initially start off with 3 – 4 short bouts of 5-10 minutes each. If you’re more fit, then you might go for 10 – 20 minutes each for 2 – 3 times.
And if you already have a reasonable fitness base, then you may want to go straight into 40+ minutes of continuous activity.
Take home message
- Hyperinsulinemia is characterised by high levels of insulin in the blood and is often a reflection of the degree of insulin resistance.
- There are generally no signs or symptoms, but they may occur in the presence of accompanying high blood sugar (hyperglycemia).
- Because hyperinsulinemia is associated with a number of other disease states, it is important to treat the underlying cause so it doesn’t progress to other conditions.
- Lifestyle changes are powerful medicine for improving insulin sensitivity, reducing insulin resistance, improving blood sugar control, and reducing hyperinsulinemia.

Good Morning,
In my search for information on my recent Sugar Alcohol Binge, I ran across this article, Love It!!
Briefly, I have reactive hypoglycemia or hyperinsulinemia, not sure which.
I rarely consume sugar alcohols, however, recently binged on chocolate candy sweetened with sugar alcohols, specifically, Maltitol & Maltitol Syrup. The fact is I ate approx 35 pieces of the candy, almost all in one sitting. I am now on day 5 of feeling horrible, can’t seem to shake it. Do you have any suggestions for quicker relief of the symptoms, the gastro symptoms lasted one day, the balance of symptoms….short of breath, moody, massive hunger, weak, tired, shaky, etc are continuing. I feel like I totally threw my system out of whack and can’t seem to return to normalcy.
I’d suggest consulting your doctor for a proper evaluation and work up. That would be you most prudent first course of action.
Hello Dr Sukala,
I am a 77 year old male living in Australia. I have had Diabetes Type 2 for about 20 years, plus all the issues that precede it including hyperinsulinemia. I have been learning about hyperinsulinemia and insulin resistance recently, but realise now that I have had these conditions for many decades. My BP was 120/80 at age 17, but I had developed high blood pressure by age 21. I started medication at age 24, and have been on it continuously since then. My diet between ages 17 and 24 was quite unusual. I was living with my father during those years, and he gave me the same meal EVERY single day. It was rump steak, boiled potatoes smothered in butter, peas or green beans, and carrots. Two eggs on toast for breakfast. Plus he started me on tea and coffee with sugar. No source of omega-3. Plus a lot of stress from living with my eccentric father and from striving hard to do very well at University. Do you think that these factors could have caused me to have hypertension this early in life? I have often tried to get off meds (metformin) over the years, but nothing works.
My main reason for this post is to say that I found your information on this page to be the very best and most comprehensive I have found. Although I have read a lot of information lately, I still had new or deeper realisations after reading your above article. For example, WHY exercise helps to lower blood pressure. Thank you so much for posting the above article.
I am eating in a fairly healthy way now, a vegetarian diet, but just cannot force myself to do much exercise at all. Maybe the information above will help to motivate me. Do you have any additional suggestions for how to motivate myself to do more exercise please?
Kind regards,
Richard
Hi Richard,
Thanks for your comment and for sharing your story. When looking back many decades, it’s hard to know exactly where things went a bit haywire. It’s possible things could have been set in motion back in your early 20s, but I suppose we’re only left to speculate on that. But in general, as we get older and tend to see a reduction in muscle mass and an increase in stored body fat, this combination changes the overall metabolic chemistry of the body and can lead to downstream effects on inflammation and eventually interrupting normal insulin signalling and causing disruptions in blood sugar levels.
One thing we know with certainty is that hyperinsulinemia isn’t a one trick pony and there are often a variety of factors that are playing into it. Reversing this, or at least controlling it to some degree, often comes from the ugly / boring advice to alter the diet and add in exercise. It sounds like you’re on the right track with upping your veggie intake. All those powerful plant chemicals have a positive effect on your body’s overall chemistry (in particular, reducing inflammation etc). Exercise can be a slog for a lot of people, but ultimately it comes down to trying to identify activities you enjoy or can incorporate into other things like social groups. If you’re located here in Sydney, I know as a matter of fact that there are a lot of local social groups doing trail walks and things. Not sure if that’s your cup of tea, but the thing I like about that idea is that the focus is on social engagement and the exercise comes automatically in the background without having to view it as a slog.
In general, if you enjoy other activities and can weave them into a social setting, that can really help with the motivation side of things (when people know you and are expecting to see you there).
If you wanted to get into resistance training / weight lifting, that can also have potent positive effects on helping control your insulin and glucose levels. But if you’re on a cocktail of medications, exercise can potentiate their effects and possibly lead to your blood sugar going too low. So you will want to work with your medical management team to see about how to fit in exercise safely.
Hope this helps move you in the right direction.
Kind regards
Bill