Obstructive Sleep Apnea (OSA) in adults has been well documented in Australia, the United States, Europe, and Asia.
Studies have shown that approximately 1 in 5 adults have a mild form of OSA and 1 in 15 has moderate or severe OSA.1 These statistics should make you take note of your own sleep health.
So could YOU have sleep apnea and how can you know for sure?
What is sleep apnea?
First let’s take a look behind the scenes. What exactly is sleep apnea? Sleep apnea is an obstruction of the upper airways affecting normal breathing and respiration while sleeping. This is known as Obstructive Sleep Apnea (OSA).
Periodically and repetitively during sleep, your airway is blocked (minimal to zero airflow) by the collapsing of soft oral tissue such as the tongue, soft palate, pharyngeal wall and/or the uvula.
Breathing can stop for at least 10 seconds before your brain signals your body to temporarily wake and “jump start” your normal breathing again – you often have no recollection of these episodes in the morning.
These disruptions in your normal sleeping pattern often throw you out of the deeper sleep stages (known as wakefulness and arousals) and impede your ability to obtain a good night’s sleep.
Related article: Under Armour Athlete Recovery Sleepwear Review
Why is it such a problem?
Adequate sleep is vital for optimal functioning of your body’s biochemical processes but may become compromised in the setting of sleep apnea. Long term intermittent hypoxia (deprivation of adequate oxygen) can result in:
- reduced oxygen saturation (can sometimes fall below 60%)
- increased blood pressure
- systemic vasoconstriction (your blood vessels tighten)
- retention of carbon dioxide
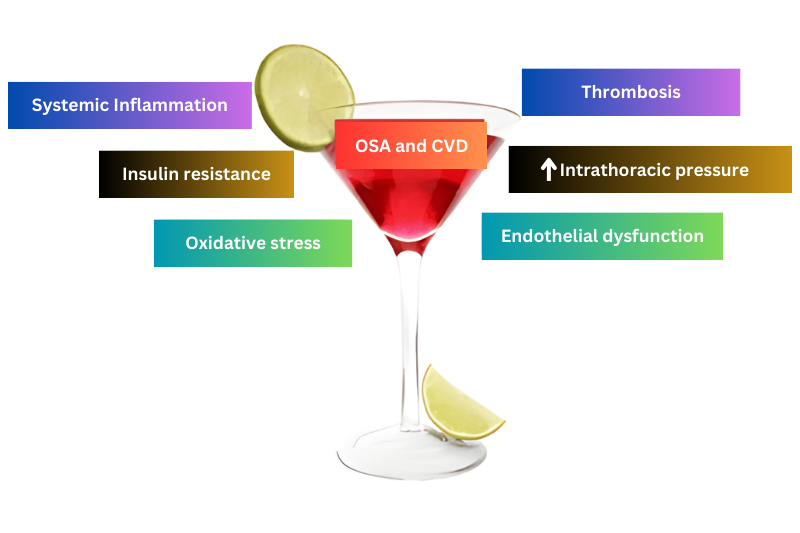
These responses may act to promote cardiovascular disease.2, 3 Figure 1 illustrates the potentially harmful cocktail of factors linked to sleep apnea which may contribute to the development of CVD.
What are the risk factors for sleep apnea?
Some of the known risk factors for obstructive sleep apnea include:
- Obesity: Body mass index of greater than 25kg/m2 accompanied by a large neck (>43cm for men and >40cm for women) and waist circumference (>94cm for men or 80cm for women) – present in more than 60% of patients referred for diagnostic evaluation.4
- Physical Inactivity: Lack of exercise and physical activity is associated with increased severity of sleep-disordered breathing and obesity. Studies have shown that participating in aerobic or recreational activity 3 days per week for at least 30mins per day (60-70% peak VO2) and including resistance training 2 days per week may exhibit a protective effect on the severity and occurrence of OSA.7
- Existing Chronic Condition: Some existing chronic conditions can facilitate the development of OSA usually via long term respiratory stress and effort. These may include hypertension, diabetes, heart failure, existing pacemaker, asthma, and chronic obstructive pulmonary disease COPD.1
- Gender: Men have a higher propensity due to various factors such as obesity pattern and fat distribution, upper-airway anatomy and function, the control of breathing, and hormone status.8,9 More research needs to be done to conclusively define male gender as an independent risk factor for apnea.
- Age: 65 years of age or older. There is a natural reduction in the muscle tone of the oral soft palate, pharyngeal wall, and uvula during aging. More than 50% of people of age 65 years have reported some form of chronic sleep disorder complaint.4
- Family history: Individuals with a family history of OSA or sleep-disordered breathing are more susceptible than those without a familial link.4
- Facial abnormalities: Certain facial structural abnormalities, including a high, narrow, elongated, soft palate, a small chin, an abnormal bite, and a small jaw can predispose you to sleep apnea.4
- Vices: Cigarette smoking and excessive alcohol consumption increases the likelihood of developing OSA.4 Initially alcohol may act as a sedative but several hours later elicits periods of wakefulness and arousal. The relaxation effect of alcohol can also exacerbate OSA by increasing the laxity in oral soft tissue. The National Health and Medical Research Council recommend no more than two standard drinks per day for both male and females.
- Medications: Certain medications may affect respiratory architecture and breathing. Medications such as sleeping tablets or sedatives, benzodiazepines (anti-convulsive and/or anti-anxiety) and opiates (pain relief) aid in relaxation. These pharmacological offenders suppress breathing and make the soft tissue of the upper airway more collapsible.5,6
What are the signs and symptoms of sleep apnea?
It is often the bed partner of a sleep apnea sufferer who first recognizes symptoms. Here’s a checklist of the most common indicators of OSA:
- Chronic snoring
- Waking gasping for breath
- Witnessed apnea (frequent pauses in breathing whilst asleep)
- Excessive daytime tiredness and fatigue
- Waking unrefreshed
- Dry, sore mouth and/or throat
- Irritability and mood changes
- Frequent urination during the night
How is sleep apnea diagnosed?
Sleep apnea in Australia and the United States goes largely undiagnosed. In fact, since more than 85% of patients with clinically significant and treatable OSA have never been diagnosed,1 it makes sense that most people with sleep apnea are often unaware they have it.
First line evaluation may include the Epsworth Sleepiness Scale, a self-report questionnaire designed to identify daytime tiredness and lethargy. Positive results may not indicate a confirmed diagnosis but the questionnaire encourages further investigation via a sleep study assessment.
A definitive diagnosis of sleep apnea can be made only with a sleep study conducted during a visit to a sleep lab – usually overnight – or a home study performed with special equipment (and if used by an experienced clinician).4 This is called a polysomnogram.
How can I take action against sleep apnea?
The good news is you can manage sleep apnea. If you’re experiencing signs and symptoms and think you may have it, consult your doctor for referral to a qualified sleep physician and a diagnostic sleep assessment.
The earlier you take action the better the long term outcomes for reducing the potential for adverse cardiovascular, metabolic, respiratory, and psychological effects.
Where can I get more information?
More information can be found on the Sleep Health Foundation website.
In the United States, The American Academy of Sleep Medicine has a sleep health information resource online at https://www.sleepeducation.com/
References
- Mugnai, G. (2010). Pathophysiological links between obstructive sleep apnea syndrome and metabolic syndrome.Giornale Italiano di Cardiologia (Rome). 11(6): 453-9.
- Somers, V.K., Dyken , M.E., Mark, A.L., Abboud, F.M. (1993). Sympathetic-nerve activity during sleep in normal subjects. New England Journal of Medicine. 328:303-307
- Somers, V.K., Dyken, M.E., Clary, M.P., Abboud, F.M. (1995). Sympathetic neural mechanisms in obstructive sleep apnea. The Journal of Clinical Investigation. 96:1897-1904
- Punjabi, N.M. (2008). The Epidemology of Adult Obstructive Sleep Apnea. Proceedings of theAmerican Thoracic Society.5(2), 136-43.
- Guilleminault, C. (1990). Benzodiazepines, Breathing, and Sleep. American Journal of Medicine. 88 (suppl 3A): 25-28
- Teichtahl H, Wang D, Cunnington D, et al. (2009). Hypoxemia in patients on chronic opiate therapy with and without sleep apnea. Sleep Breath. 13: 49–57. 41.
- Silva, R .P., Belli, K.C., Carissimi, A., Fiori, C.Z., Faria, C.C., Martinez, D. (2011). Are there benefits of exercise in sleep apnea? Sleep Science. 4(2):61-67.
- O’Donnell, C.P., Schwartz, A.R., Smith, P.L. (2000). Upper airway collapsibility the importance of gender and adiposity. American Journal of Respiratory Critical Care Medicine.162(5):1606-7.
- Schwab, R.J. (1999). Sex differences and sleep apnea. Thorax. 54(4):323-8.


Lana Eyeington
Wednesday 7th of January 2015
Thanks for your comment Donald. I agree, gasping and witnessed apneas are classic signs of obstructive sleep apnea and should encourage seeking medical advice as soon as possible. In most cases it is the bed partner, friends or family that notices symptoms first, and effectively become the "eyes and ears" for sleep physicians. You knew something was wrong, you sought medical advice and now your wife's sleep apnea is being successfully treated. However, we can't self diagnose and begin treatment without the appropriate medical work-up.
I do believe the study that diagnosed your wife's sleep apnea was more than just numbers. By "a definitive diagnosis" I mean a diagnosis that is made by a qualified sleep physician after an extensive workup, on which the CPAP therapy is based. This entails a detailed medical/sleep history and an overnight sleep clinic Polysomnography (PSG) study which assesses brain activity/sleep staging, respiration, leg/jaw movement, heart rhythm, blood oxygen and body position.
With this information the sleep physician can answer such questions as what sleep stages are obstructive sleep apnea and snoring most severe? Is the patient getting enough deep sleep (Stage 3, REM sleep)? What sleeping position is the sleep apnea more severe? What CPAP pressure is required for sleeping on your back vs sleeping on your side?
Yours in health,
Lana Eyeington, MS, BS(hons) Clinical Exercise Physiologist Sleep Scientist
Donald Lewis
Sunday 4th of January 2015
"A definitive diagnosis of sleep apnea can be made only with a sleep study conducted during a visit to a sleep lab – usually overnight – or a home study performed with special equipment" I disagree. I was confident in my diagnosis of my wife's (now treated) sleep apnea. Pretty clear cut when her breathing stops repeatedly all night long and when it starts she is gasping like she is dying! The study provided numbers and prescription for CPAP, but I KNEW something was wrong.